According to one study, residential rehabilitation can indeed spur positive outcomes—although the journey isn’t the same for everyone
This post is reprinted with permission from one of TreatmentMagazine.com’s go-to blogs about addiction, treatment and recovery: Recovery Review.
By David McCartney
Recovery journeys are dynamic, take time and may need several episodes. For some, residential rehab is part of the journey, just as harm reduction interventions can also be part of the journey. However, residential rehabilitation is a complex intervention, and complex interventions are difficult to study.
In Scotland, the government is making rehab easier to access and growing the number of beds. This development is not without its critics. Some feel the resource needs to “follow the evidence”—in other words, into harm reduction and MAT interventions. This all-the-eggs-in-one-basket position would reinforce the rigid barriers that make rehab the domain of the wealthy or the lucky.
“Follow the evidence” in this context is a refrain that implies there is no evidence that rehab works to help people achieve their goals and improve their quality of life. That is simply not true. Last month saw the publication of a literature review on residential rehab by Scottish Government researchers. It’s a thorough piece of work. This summary of the research evidence provides verification that “that residential rehabilitation is associated with improvements across a variety of outcomes relating to substance use, health and quality of life.”
What happens within the walls of rehabs is diverse and the models and delivery vary, so when we talk of rehab we are not talking about something uniform.
Rehab is linked to improvements in mental health, offending (that is, criminal justice involvement), social engagement, employment, reduction in substance use, and abstinence. There is little research that compares rehab with other treatments delivered in the community, but where there is, the evidence suggests that “residential treatment produces more positive outcomes in relation to substance use than other treatment modalities.” The review also suggests that rehab can be more cost-effective over time than other treatments.
The report also highlights problems and gaps in the evidence base. What happens within the walls of rehabs is diverse, and the models and delivery vary, so when we talk of rehab we are not talking about something uniform. We need to gain an understanding of the most effective interventions. Research suggests, for instance, that integrating mental health care into rehab treatment is associated with better outcomes.
The Scottish Government’s literature review highlights gaps that need to be plugged. I think it’s fair to say that there are no queues of Scottish academics curling around the block—researchers champing at the bit to get their teeth into studies on the place of rehab in treatment and recovery. That we have unanswered questions is not a surprise. Further, it’s important for us to face up to the fact that rehab is not necessarily without risks to individuals, particularly for those with opioid dependence. Those need to be faced head-on.
Indeed, the perception of such risks may be one of the main reasons for resistance to rehab as an intervention. We don’t know whether in Scotland those going to rehab have higher mortality than in other kinds of treatment, but there is evidence from elsewhere that this could be the case. However, it is plausible that people with higher problem severity (and higher risk of death as a result) end up in rehab. The mortality rate in intensive care units is higher than in general wards, but we don’t stop people from going to intensive care because of that.
Recovery housing, take-home naloxone, overdose prevention, assertive referral into recovery community resources, outreach and recovery checkups may also reduce risks. Standards could be developed to encourage the adoption of such practices.
We also need to be aware that there are mitigations that can be employed to reduce risks. These may include things like comprehensive aftercare, re-titration of those who want to leave treatment early, and rapid re-entry into prescribing services if individuals return to use.
Recovery housing, take-home naloxone, overdose prevention, assertive referral into recovery community resources, outreach and recovery checkups may also reduce risks. Standards could be developed to encourage the adoption of such practices. The impacts of these have not been tested in research, but they could be.
I don’t believe it is in the interests of those individuals (and their families) who struggle with dependence on substances for us to maintain treatment turf wars. We can have harm reduction and recovery. We can have MAT and abstinence. We can have outpatient treatment and residential rehab. Whatever we have, it needs to be plugged into supports across housing, criminal justice, benefits, education, training and employability, and health. A joined-up, comprehensive treatment system with strong links between its component parts will serve individuals best.
Evidence suggests that over a lifetime, most people resolve their problematic use of substances.
We don’t need to say that one thing is better than another, but we do need choice, and through shared decision-making we can try to help patients align themselves to a treatment option that helps them meet their goals. And we need to be humble too. Evidence suggests that over a lifetime, most people resolve their problematic use of substances. When they look back, they may be grateful for the part that treatment played in their recovery, but it is likely that it will be only one of many factors that helped.
For the moment though, we can certainly challenge the voices that say “there’s no evidence that rehab works,” for there is ample evidence that it does. I’m not unrealistic about this though. As I’ve been writing, I have been mulling over the wisdom of Ahmed Kathrada’s observation: “The hardest thing to open is a closed mind.” That shouldn’t stop us trying.
This Recovery Review post is by David McCartney, who is an addiction medicine specialist and Clinical Lead at LEAP, a quasi-residential therapeutic community addiction treatment program in Scotland. He trained as a family medicine practitioner and spent much of his career in practice in inner-city Glasgow. Having retrained in addictions, he now works exclusively in the field and until recently was an advisor to the Scottish government on drug policy. He is a member of the Royal College of General Practitioners. His opinions expressed here don’t necessarily represent the views of his employer. Find more of his writing, as well as a thought-provoking range of articles, insights and expert opinions on treatment and addiction, at RecoveryReview.com.blog.
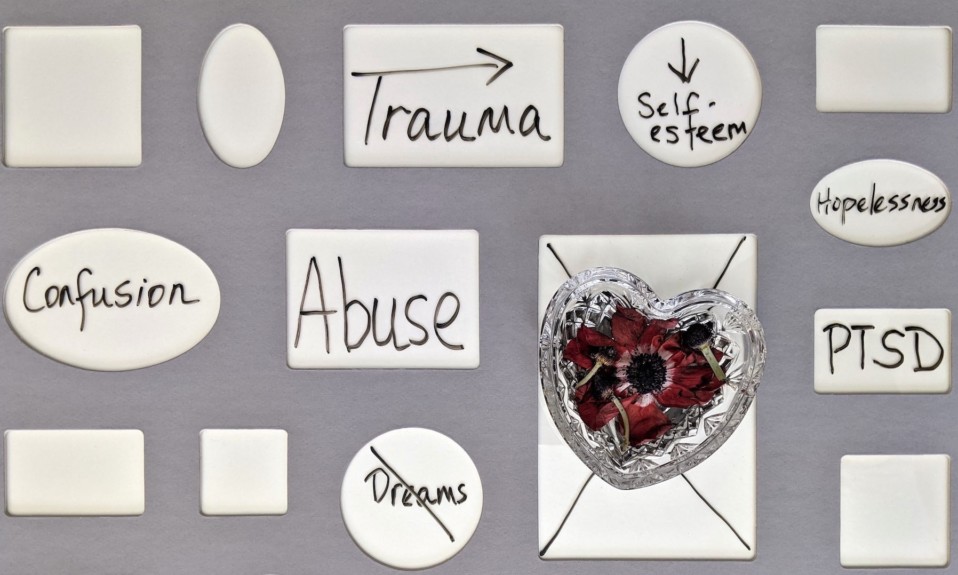
Photo: Chris Henry