This treatment approach strives to keep people struggling with substance abuse alive long enough to help them get treatment and care
By Jason Langendorf
November 17, 2020This look at Harm Reduction is part of a regularly published “Addiction Therapy Spotlight” series by TreatmentMagazine.com looking at the spectrum of treatment recovery approaches and models.
One of the core tenets of the physician’s Hippocratic Oath states, “First, do no harm.” But for clinicians in addiction and treatment, what if it turns out the current standard approach to treatment—abstinence as a baseline—inadvertently does more harm than good?
That’s the question asked by proponents of harm reduction, a somewhat polarizing but increasingly popular approach to improving outcomes for substance users. For those who champion the principles of harm reduction, the answer is conclusive: The long-accepted corrective measures applied by our various substance-control entities—recovery facilities, hospitals, legislative bodies and the criminal justice system—have been not only ineffective, but rather a driving force behind America’s drug epidemic.
The facts are grim: Since 1999, more than 750,000 people in the United State have died from a drug overdose. Of those deaths, the cases involving opioids have increased almost six times during that span. Abuse of tobacco, alcohol and illicit drugs is estimated to cost the United States more than $740 billion annually. Of the more than 1.2 million Americans arrested for a drug abuse violation in 2018, 27.1% were Black—despite being only 13.4% of the U.S. population.
Harm reduction is the connection point. That’s what I saw when I first started practicing. It’s like, ‘Wow, these people that have already been marginalized for a whole bunch of reasons are now becoming connected to services.’ It’s that real ability to connect people.”—Emma Roberts, senior director at the National Harm Reduction Coalition
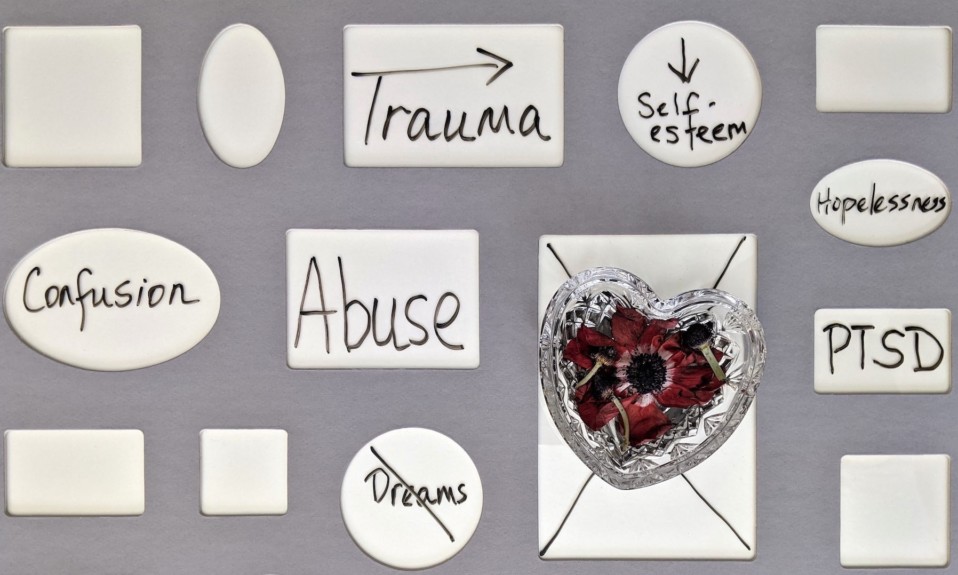
The emergence of harm reduction arguably was a response to that multiplying human and financial toll. Its premise is just like it sounds: reduce harm. By supporting and remaining open to a variety of strategies that help lessen the consequences associated with substance abuse, advocates of the approach hope to rethink what success looks like in addiction treatment.
“In harm reduction, we’re broadening the definition of recovery,” says Emma Roberts, senior director at the National Harm Reduction Coalition. “Because if anything, what we’ve learned from data in the research is that that narrow definition is only working for somewhere between 10 to 20% of people who struggle with drug use. So what are we doing for the other 80 to 90%?”
Access is critical, but research has shown that many people who use substances don’t try to access addiction care for a number of reasons, including stigma and an unwillingness to stop using. Harm reduction attempts to address these issues by meeting people who use drugs on their own terms, connecting but not coercing, supporting without judgment. Although definitive research on the efficacy of harm reduction is thin, especially in the United States, anecdotal evidence is beginning to pile up that suggests this flexible, humanistic approach gets results.
“What we want is for it to work,” says Roberts. “We want more options to work for more people, more of the time. It’s recognizing that the system is something that we’ve done since the beginning of time, and also that the way we criminalize and stigmatize people is a social construct, one that’s been constructed over a long history.”
How Does Harm Reduction Work?
The components of harm reduction can take many forms, ranging from syringe exchange programs to medication-assisted treatment (MAT) to non-judgmental psychotherapy. Empathy and therapies that fit within the context of a person’s circumstances and preferences are a guiding principle. Sobriety? A therapist will help a patient toward that goal if they wish, but there are no requirements or expectations.
In a 2014 review of harm-reduction research conducted by Diane E. Logan and G. Alan Marlatt, whose work was on the leading edge of the subject, the authors outlined a helpful example: “If a client presents after one month of treatment and reports consuming five drinks on each of the past three nights, a traditional program would count that as a failure. If abstinence was required for certain services, including housing, that client may be turned away from further treatment. Alternatively, a harm reduction practitioner would first ask how much the client drank at the beginning of therapy. If the client were drinking 10 drinks every day, then the consumption of five drinks a day would be a therapeutic success, or steps in the right direction. If the client’s goal were to abstain, then the therapist would continue to work with the client to troubleshoot the problematic areas and develop other coping skills.”
Harm reduction can take many forms, ranging from syringe exchange programs to medication-assisted treatment (MAT) to non-judgmental psychotherapy. Empathy and therapies that fit within the context of a person’s circumstances and preferences are a guiding principle.”
Even for those who don’t necessarily consider abstinence to be a moral imperative, however, failing to hold accountable users of hard drugs may smack of a fanciful naivete—or negligence. No matter that, for instance, needle programs have demonstrated they help protect police officers as well as those who use, or that medications such as naltrexone, buprenorphine and methadone have been proven effective in reducing relapse incidence. Critics argue that these harm-reduction tactics condone and perhaps even encourage a culture of substance abuse. That some of the programs are funded by taxpayer dollars only fuels further outrage for some.
But it’s the villainization of substance use, says Matt Sutton, director of media relations at the Drug Policy Alliance, that perpetuates the very behavior hard-liners claim to be fighting against.
“As we know, criminalization does not help people who are struggling with drug use, who have an addiction,” Sutton says. “That’s the common misconception that we’ve dealt with—that public officials and prosecutors have put out this idea, this messaging that if less people are arrested for their drugs, they’re not going to get the help that they need. Which is just not true. What we’ve seen is coercive treatment, even when it is offered—and more times than not, it’s not offered; whatever resources available through the jail or prison or community supervision programs is very, very minimal. When people are forced into it, it ends up being not effective.”
The History of Harm Reduction
The origin of harm reduction as a substance-use intervention dates back at least to the 1980s, when needle-sharing among users of intravenous drugs gave rise to the HIV epidemic. By the time the National Harm Reduction Coalition was founded in New York in 1993, a number of countries in Europe—Holland, the Netherlands and Portugal, for instance—were already learning about the effectiveness of harm-reduction methods in reducing the transmission of HIV and hepatitis B and C.
Criminalization does not help people who are struggling with drug use, who have an addiction.”— Matt Sutton, director of media relations, Drug Policy Alliance
In the years since in the United States, the success of local syringe exchange programs and law enforcement diversion programs have demonstrated they help substance users stay healthier and out of jail. Given the estimated costs for lifetime HIV treatment (more than $400,000 for a single individual) and the federal outlay for punishing drug offenders ($10 billion annually), even a stone-cold capitalist can find good reason to get behind the harm-reduction movement.
The Value of Harm Reduction & Connection
For Roberts and other harm reduction advocates, any cost savings reaped is incidental when compared to the value in bridging the gap between people struggling with substances and healthier, fairer, more-stable environments. She makes an important distinction. “It’s not a therapy,” she says, emphasizing how harm reduction can be incorporated into most any form of therapy. Roberts further notes the significance for those at risk of being failed by a system that has let down so many others.
“They’re pushed away and they don’t feel connected,” Roberts says. “They don’t feel capable of succeeding. Harm reduction is the connection point. That’s what I saw when I first started practicing. It’s like, ‘Wow, these people that have already been marginalized for a whole bunch of reasons are now becoming connected to services.’ It’s that real ability to connect people.”
Photo: Clay Banks