That’s no easy task—he talks a mile a minute—but we absorbed plenty of insights from one of the field’s great thinkers
By Jason Langendorf
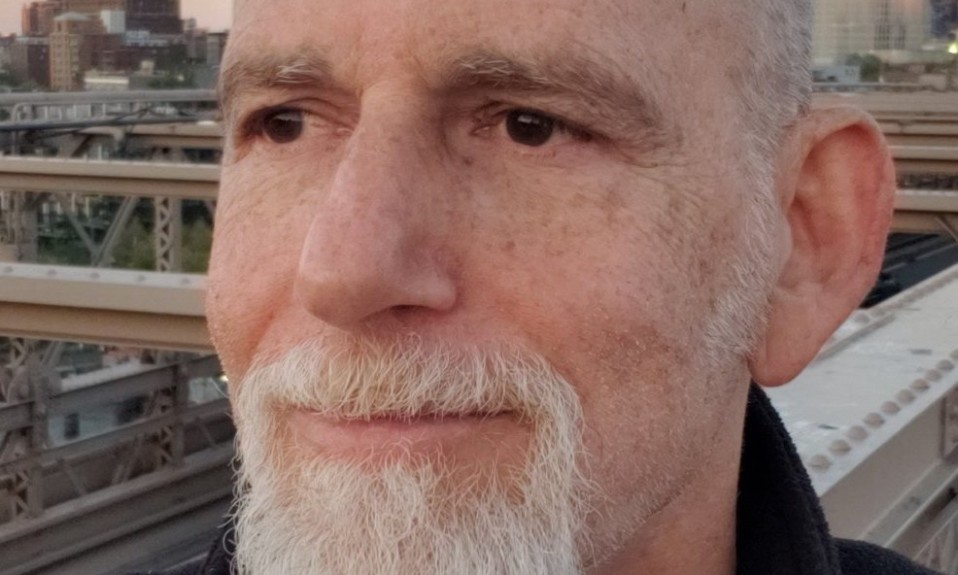
After a four-year professional hiatus, Ethan Nadelmann, the founder and retired executive director of the Drug Policy Alliance (DPA), is again tackling issues of addiction and treatment policy as the creator and host of the new podcast Psychoactive.
Nadelmann, 64, was drawn to drug policy as a student at Harvard, where he began publishing articles on the subject, gained federal security clearance, traveled to dozens of countries and conducted extensive interviews within key drug enforcement and law enforcement agencies that led to his authoring two books (Cops Across Borders: The Internationalization of U.S. Criminal Law Enforcement and Policing the Globe: Criminalization and Crime Control in International Relations). As a professor of politics at Princeton, he became increasingly interested in the drug reform movement and in 1994 he founded the Lindesmith Center, a drug policy institute that would later become the Drug Policy Alliance.
TreatmentMagazine.com spoke to Nadelmann, once described by Rolling Stone as “the real drug czar,” about his new podcast, America’s complicated relationship with substances and where U.S. drug policy is headed.
Q: What was behind your decision to create Psychoactive?
A: Well, when I stepped away from DPA [in 2017], I literally just wanted to stop talking about drugs for a while. I mean, I would take a brief vacation, and somebody would ask me what I did for a living. I’d say, “I can’t tell you,” because the issue is so inherently interesting that everybody’s always got an opinion. They’ve always got personal experience. So I just needed to kind of cut back. But I will say, I started getting a bit restless, especially during the pandemic, wanting to re-engage and feeling like this drug issue has been in my bones—not just drug policy, but thinking about drugs and drug history and drug cultures and drug markets. Since I was 18 and first smoked a joint, and since I was in my early 20s, when I started researching this issue.
So out of the blue, I get an email from Darren Aronofsky, the movie director. I’d met him maybe 16, 17 years ago, and then I would see him on a couple of occasions. He runs this movie production company called Protozoa, and they were looking to make a deal with iHeart Radio so that he can make not just movies but podcasts. He thought of me and sent me an email: “Hey, man, you want to do a podcast on psychedelics?” And I said, “No, I want to do a podcast on all drugs!” And he said, “OK, let’s do it.” So we’ve been working on it, and I’m loving it. I’m back working with people half my age, which is one of the things I miss from stepping down from DPA.
Q: Who are some of the guests you’ve booked for Psychoactive so far?
A: The next episode will be [author] Dan Savage. I didn’t know him before, and that was a fun one. I got Nora Volkow, the head of NIDA [National Institute on Drug Abuse]. She pleasantly surprised me by accepting my invitation. I grilled her pretty hard, but she was gracious. I got Kate Nicholson, who heads this organization about people who are being prescribed opioids for chronic pain and using them successfully but who are now being stigmatized and can’t even find doctors to treat them, because doctors don’t want to deal with those people. I interviewed Clive Bates, who is probably the world’s leading expert on issues of tobacco harm reduction. I’m doing an interview with Larry Krasner, the district attorney of Philadelphia. I interviewed the former President of Colombia, Juan Manuel Santos, who won the Nobel Peace Prize for helping to resolve the civil war there. He was a real courageous leader on the drug issue. I had Patt Denning, who is one of the most thoughtful harm reduction writers and teachers in the country, out of San Francisco. I interviewed a professor at Columbia, Carl Hart, who wrote that book Drug Use for Grown-Ups and used to be on my board at DPA.
I also interviewed a colleague of his at Columbia, Elias Dakwar, who has done some really fascinating government-funded research on using a combination of ketamine and mindfulness meditation in helping people who have drug addictions. I have Tim Ferriss, who has his own business podcast with millions of listeners; he’s been very involved in the psychedelics area. I interviewed my former colleague, Melissa Moore, who directs advocacy efforts in New York for the Drug Policy Alliance. That was fascinating—I got to her just shortly after they won that victory.
Q: Is the idea to interview a wide cross-section of voices on the issues?
A: Yeah, everything from celebrities to activists to people who have had traumatic experiences with drugs, to people have had remarkable experiences with drugs. I wanted the episode with Andy Weil to go first because he and I go way back, since 1987, and he was a major influence on me. But also because of his framing of the issue: He says there’s no such thing as good or bad drugs, only good and bad relationships with drugs. That’s a beautiful frame for what this show is about. It’s really about understanding there are cultures that are more successful in dealing with all drugs or some drugs than others. There are people who are more successful than others. There are all sorts of reasons for that. America, you know, we’re not the worst in the world when it comes to drugs. But we are the worst in the world when it comes to locking people up.
We live in a pill-popping culture, and we live in a culture where doctors are under pressure to spend minimal time with patients, and we live in a culture where doctors and nurses and others aren’t really trained in pain management.”—Ethan Nadelmann
Just look at the history of alcohol. We go from this place where alcohol is everywhere to alcohol prohibition and generating Al Capone and crime and violence and corruption and black markets and more dangerous drugs. And then we come out of it, but we Americans have a hard time finding that balance between the free market promotion and the moralistic punitive prohibition. And I’ve done enough studying of other societies, as well as some instances in American society, where sometimes we succeed in doing things better. So this is about policy, but it’s also about people’s personal lives.
Q: Do you envision a future in America when drugs are de-stigmatized and properly regulated, and there’s that “healthy relationship” you described earlier?
A: I do, I do. I’m pretty confident. Right now we’re headed mostly in the right direction, I think, on cannabis, on psychedelics and on decriminalizing any drug. And because of COVID, we’re getting smarter about making methadone and buprenorphine more readily available to people having a problem with street opioids. On the other hand, fentanyl obviously is scary, and we need to get a handle on that in a lot of different ways. It’s not going to be a supply-side approach, because what do you do with a drug where a little box that can overdose thousands or tens of thousands of people can come through the mail or FedEx?
But the Oregon ballot initiative—there were two; one was on psychedelics reform, and the other one was on drug decriminalization. And it was basically saying, “Let’s try the Portugal model in the U.S.,” which is, ‘We’re going to make a commitment to not putting people in jail for possession of small amounts of any drugs, including the ‘hard drugs.’” We’re going to increase access to harm reduction and drug treatment services; we’re going to shift money that way. There have been a lot of inquiries about how to do the Oregon thing, so there’s going to be more drug decriminalization ballot initiatives popping up in the next few years in different states; there’s going to be bills being proposed in state legislatures. There was a bill that was just proposed in Congress last week on all drug decrim. And when they say decriminalization, what it really means is treating drug use and possession as a health issue. All the evidence that we have from Europe and elsewhere is that doing that does not appear to present any risk of more people using drugs. If anything, it helps facilitate people getting the help they need. It means that people are using drugs and not being [targeted by] the authorities or getting in trouble; they’re just left alone. And it means that people who are having some problems can get help. I mean, that’s the basic idea that you want.
The challenge is not how to get rid of drugs, because that cannot be done. We’re never gonna be a drug-free society. … The challenge is to learn how to live with drugs so that they cause the least possible harm and, in some cases, the greatest possible benefit.”—Ethan Nadelmann
So I think the criminal justice reform side of things is very promising. But it’s very hard to see drugs like heroin, cocaine and methamphetamine actually getting legalized in the way alcohol is or the way marijuana is now becoming. Even as support for legalizing marijuana went up from 30% 20 years ago to 60, 70% now, we didn’t see any real change in people favoring the legalization of all drugs. As for psychedelics, I don’t think we’re gonna see any sort of big over-the-counter sales—maybe microdosing or something like that. But that’ll be much more about making it available in a therapeutic context.
Q: At the end of the day, are we capable of harnessing the effects of drugs while still protecting the public against their risks?
A: When the opioid thing started to get out of control, it made me begin to think seriously about this—and I’ll lay this out in future episodes. We have an epidemic of pain. I mean, there really are just massive forms of pain here. Huge numbers of people struggling and suffering—both among the impoverished and people of color, but also among white people who aren’t doing as well as their parents or grandparents, for all sorts of reasons. It’s hard. We live in a pill-popping culture, and we live in a culture where doctors are under pressure to spend minimal time with patients, and we live in a culture where doctors and nurses and others aren’t really trained in pain management.

So, one of my theories about what’s going on with the opioid epidemic is that some significant portion of that pain people are seeking opioids for, both legally and illegally, is actually not something wrong with their physical bodies. It’s more about a form of existential or emotional pain that’s not being processed and is being effectively converted into physical pain in ways that are hard to believe, because it’s hard to believe that emotional pain could cause that much physical pain unless there’s something wrong in your body. What I also found was that opioids don’t work that well for pain that is essentially emotional in its origins. I mean, if you inject something one time in an emergency room—an injection of Demerol or whatever—yeah, shit, that’s going to take away all the pain you feel for a while. But you build up a tolerance to that fast, and then opioids don’t work as well for that kind of stuff.
So, how do we make drugs available in ways that benefit people without opening up the doors to much bigger problems with drug abuse? That is the $64,000 question. When I was teaching 30 years ago, that was the question. I’ve often framed my overall thinking, both at the DPA and now with the show, in two ways. One: The challenge is not how to get rid of drugs, because that cannot be done. We’re never gonna be a drug-free society; we cannot effectively build a moat between those drugs and ourselves or our kids. Give it up. The challenge is to learn how to live with drugs so that they cause the least possible harm and, in some cases, the greatest possible benefit.
More specifically, one definition of harm reduction is the policy definition—and that’s the one that says the optimal drug policy is the one that most successfully reduces both the harms of drugs use and the harms of drug prohibitionist and regulatory policies. For example, look at something like cigarettes. I’m very supportive of all these bans on smoking in different places and increasing taxes and education campaigns and all this, right? But I’m also an opponent of ever prohibiting cigarettes, because I don’t want to generate all the black market harms that we saw with marijuana or other illegal drugs. With something like marijuana, the key is, let’s stop arresting people, stop all the associated harms. We know that marijuana is the least dangerous of the popular psychoactive substances, but I know people for whom marijuana has been devastating in their lives. I know people who wake-and-bake and get screwed up. I know people who get delusional when they smoke marijuana. It’s a small percentage of people, but it exists. And I’m also concerned with some of the potential downsides of legalization. I like the fact that marijuana is now kind of being normalized in our society, but I don’t look forward to it being so normalized that people stop losing a sense of awareness or consciousness around taking cannabis.
With the psychedelics, I think right now we’re proceeding in a pretty responsible way. All these major research institutes at Harvard and Yale and NYU and Johns Hopkins and the University of California—they’re all looking at the medicinal value of psychedelics and MDMA in dealing with PTSD, anxiety, depression, addiction and what have you. I think it’s a tragedy that the federal government is barely funding any of this stuff yet, but I’m not an advocate for saying, “Let’s make high-dose LSD available over-the-counter.” Especially when you see this proliferation of synthetic substances, both psychedelics and other types of drugs that are just emerging on both the dark web and the internet, the most important thing to me is that we find sensible ways to regulate it.
With fentanyl, you don’t have to combine it with anything to stop breathing. It’s strong enough … that it’ll just knock you out. It’ll just kill you. So we have a huge interest in people who are using opioids outside the legal regulatory system. We have a huge interest in getting as many of them as possible, if they are unable or unwilling to stop now, to get their opioid from a legal supply.—Ethan Nadelmann
The last thing I would say on this is, the key now with opioids—especially before the explosion of fentanyl—is that most people don’t die of an overdose just from taking too much heroin or too much oxy. Normally, you’ve got to combine it with alcohol or benzos or tranquilizers, something like that. With fentanyl, you don’t have to combine it with anything to stop breathing. It’s strong enough—50 times the strength of heroin per microgram, or whatever—that it’ll just knock you out. It’ll just kill you. So we have a huge interest in getting people who are using opioids outside the legal regulatory system, if they are unable or unwilling to stop now, to get their opioids from a legal source.
And that’s why I’m going to make sure to have an episode about what’s going on in Vancouver, British Columbia, where they’re talking about safe supply. It’s about how you take people using street drugs daily, at dramatic risk of both various infections as well as overdose and death, and find a way to allow them to have legal access to the substance they desire without making it more broadly available to the broader community in ways that could create some greater net harm. That’s the challenge, ultimately, of drug policy.