Plus: An OUD bias among rural doctors; more grim substance stats from the COVID front; and the effects of smartphone addiction
By William Wagner
March 9, 2021Since mental illness and addiction often are intertwined, a new study out of Johns Hopkins University is particularly noteworthy: People suffering from both afflictions don’t appear to be receiving effective treatment. We also highlight the stigma attached to rural Americans with opioid use disorder (OUD), worrisome substance misuse data from the pandemic and new information about smartphone addiction.
From Psychiatry Research:
Addiction Treatment and the Mentally Ill
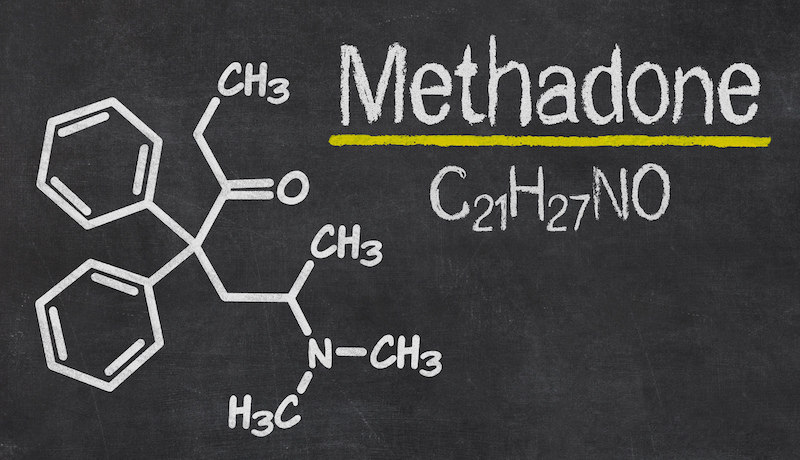
Individuals who might be most in need of addiction treatment—those who also have serious mental health issues—are least likely to get it. A research group from Johns Hopkins examined the records of 271 patients being treated for mental illness at two Baltimore mental health facilities and found they were reluctant to seek care for their addictions. For example, the patients in the study were 20 times more likely than the general population to use heroin, yet only a fraction were administered medication-assisted treatment (MAT).
The negative symptoms that accompany serious mental disorders, such as apathy, ambivalence or social withdrawal, can decrease these patients’ ability to fully participate in [addiction] treatment.”—Stanislav Spivak, M.D., Johns Hopkins University
In a news release about the research, Stanislav Spivak, M.D., assistant professor of psychiatry and behavioral sciences at Johns Hopkins University School of Medicine, said, “They may not be organized enough or may seem distracted, they may feel uncomfortable in groups or they may make other people uncomfortable. Similarly, the negative symptoms that accompany serious mental disorders, such as apathy, ambivalence or social withdrawal, can decrease these patients’ ability to fully participate in treatment.”
From Psychiatric Services:
Uncovering an OUD Bias in Rural America
The healthcare system isn’t set up to adequately treat rurally placed people with OUD. So implies a study out of Ohio University. Two professors from the university surveyed 408 board-certified physicians in Ohio and determined that doctors in rural areas are more inclined than those in urban centers to stigmatize OUD patients.
“What we know about rural opioid abuse is that if physicians rarely work with this patient population, the more bias is held,” Berkeley Franz, Ph.D., one of the Ohio University professors, said in a news release about the survey. “Physicians in urban settings, by contrast, seem to have more experience with both providing services for opioid misuse and working with that population, which may explain the lower bias that we found among this physician population.”
Franz and her colleague Lindsay Dhanani, Ph.D., plan to use the information they’ve gathered to develop an online platform that educates medical providers about bias.
From Annals of Internal Medicine:
More Research on COVID’s Impact on Substance Misuse
Data continues to flow in regarding the rise in substance misuse during the COVID-19 pandemic, this time from the University of Southern California. According to researchers from the university’s Keck School of Medicine, retail sales of alcohol and tobacco from April through June 2020 were 34% and 13%, respectively, above the same time period in 2019. They attribute the increases to the usual suspects: stress, loneliness, isolation and boredom. Treatment experts worry that these types of numbers signal an addiction tsunami in the post-pandemic world.
From Frontiers in Psychiatry:
The Effects of Smartphone Addiction
Cocaine? Really bad. Heroin? Really bad. Meth? Really bad. Smartphones? Turns out they’re not so great either. About 40% of 1,043 young adults (ages 18 to 30) surveyed by researchers at King’s College London in the United Kingdom showed signs of smartphone addiction, including sleep disorders. It’s truly an affliction for the 21st century. The team at King’s College stresses in a Frontiers in Psychiatry article that research into smartphone addiction is only getting started: “As there is continued debate concerning the possibility that smartphones may be a means to access addictive material, such as social media applications or games, rather than the addiction themselves, future research should also focus on identifying types of use associated with higher risk of smartphone addiction.”
Photo: Fernando @cferdo