The post-pandemic recovery landscape will be at least somewhat different, especially where virtual care is concerned
By William Wagner
June 14, 2020What will addiction treatment look like after we finally put the COVID-19 pandemic behind us? We’ve already had a glimpse.
As the pandemic took hold in March, spurring an economic collapse and strict social-distancing measures, many factors that lead to relapses were exacerbated. The recovery community had to move quickly to adapt, a process that is ongoing.
“Many people are struggling right now,” says Tessa Voss, MA, LADC, CADC II, executive director of the Betty Ford Center in Rancho Mirage, Calif., part of the Hazelden Betty Ford Foundation. “I have yet to find a relapse risk factor that hasn’t been amplified in this current environment. The emotional fluctuations that occur naturally during periods of great stress can be especially challenging for those in early recovery. Experiences of isolation, fear, sleep challenges, financial burdens and stress that many people have experienced during this pandemic definitely put those in recovery at increased risk.
“With that said, resiliency factors that people in recovery practice have also strengthened under these circumstances. People everywhere have found ways to connect with and support one another. We all have had to find creative ways to cope with our environment during these unprecedented times.”
Chief among those is telehealth, which has emerged as a critical tool for overcoming the isolation and various fears associated with the pandemic. In some respects, digital resources have moved the ball forward overall, actually increasing the likelihood that those in need will reach out.
“[There is a belief] that people in isolation are more likely to relapse, but I think there are lots of people who are at high risk who now are more involved in the recovery community than they were before,” says James Balmer, president of Dawn Farm, an inpatient and outpatient program in Michigan. “I know folks in the community who have struggled under other circumstances but who are active in the recovery community on a daily basis now because of having access to a computer.”
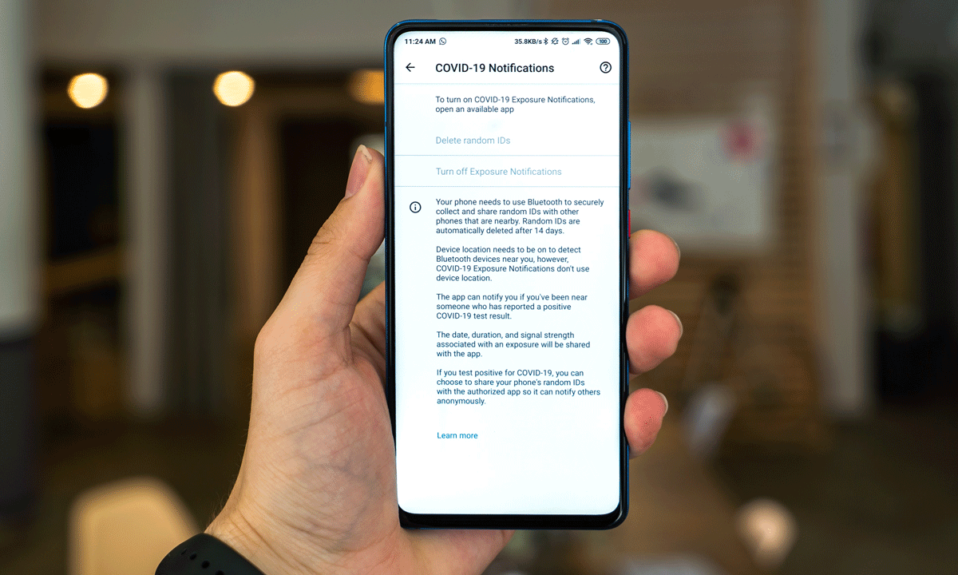
Before the pandemic, telehealth already was becoming a thing in treatment circles. COVID-19 simply has hastened its use, due in part to the loosening of restrictions surrounding virtual addiction care as part of the government’s emergency response. Boulder Care, a telehealth company specializing in treatment for opioid addiction, has been among the beneficiaries.
We have been expanding virtual care for the last year. However, our planning and implementation occurred much quicker than planned as a response to the COVID-19 crisis.”—Tessa Voss, executive director of the Betty Ford Center
“In theory, [the eased restrictions are] temporary,” Stephanie Papes, the founder and CEO of Boulder Care, told Treatment Magazine in a profile of the company. “But we’re all very hopeful that because they’re so successful and it’s driving adoption of telehealth in populations that may not have considered it before that it may become permanent even once COVID is over.”
COVID-19 has forced many treatment organizations to fast-track the development of their digital strategies, including the Hazelden Betty Ford Foundation. Hazelden’s RecoveryGo initiative provides an array of virtual services, from group and individual counseling for addicts and their families to mental health support. And when the pandemic ends, these resources will continue to be of value for individuals who have travel, scheduling or insurance limitations.
“At Hazelden Betty Ford Foundation, we have been expanding virtual care for the last year,” Voss says. “However, our planning and implementation occurred much quicker than planned as a response to the COVID-19 crisis. We are really proud of the teamwork and innovation that expanded access so quickly.”
Almost everywhere you look, you’ll find technological innovation in response to COVID-19. For example, Addiction Policy Forum and CHESS Health teamed up to launch the Connections App, which, they say, is “a free smartphone app that is scientifically proven to support patients in recovery by reducing relapse and promoting pro-social engagement.” The app aims to achieve these outcomes through features such as clinical access, a sobriety tracker and videos from a resources library.
Despite such strides, the human element—the intimacy of in-the-flesh contact—will always remain a central part of the recovery experience. Says Robert Stump, executive director of the treatment organization LifeRing Secular Recovery: “I’ve seen a very strong use of virtual meetings [during the pandemic], but it’s not the same as face-to-face. Virtual meetings are fine in terms of exposure [to the idea of recovery meetings].”
The drawbacks can extend beyond the loss of fellowship that comes from being gathered together within four walls. Virtual platforms such as Zoom, which have become widely used for meetings during the pandemic, don’t always provide the anonymity many participants seek; it’s easy, for instance, to clandestinely record meetings.
Nevertheless, there’s no turning back. COVID-19 has sent us hurtling toward a brave new world in addiction treatment.
“Addiction treatment won’t ever be the same,” Voss says. “The doors to virtual care have swung open, and it’s been remarkably successful. We have been able to reach people who otherwise may not have access to treatment.”