The annual State of Mental Health in America Report outlines how far we have to go—and what we have to do—to create a healthier nation
By Jason Langendorf
The results of a respected annual mental health study were released this month, and although they don’t include pandemic-related data, the report does reveal a general trend toward a deterioration of mental health among the population in the United States—one that existed even before the COVID-19 crisis.
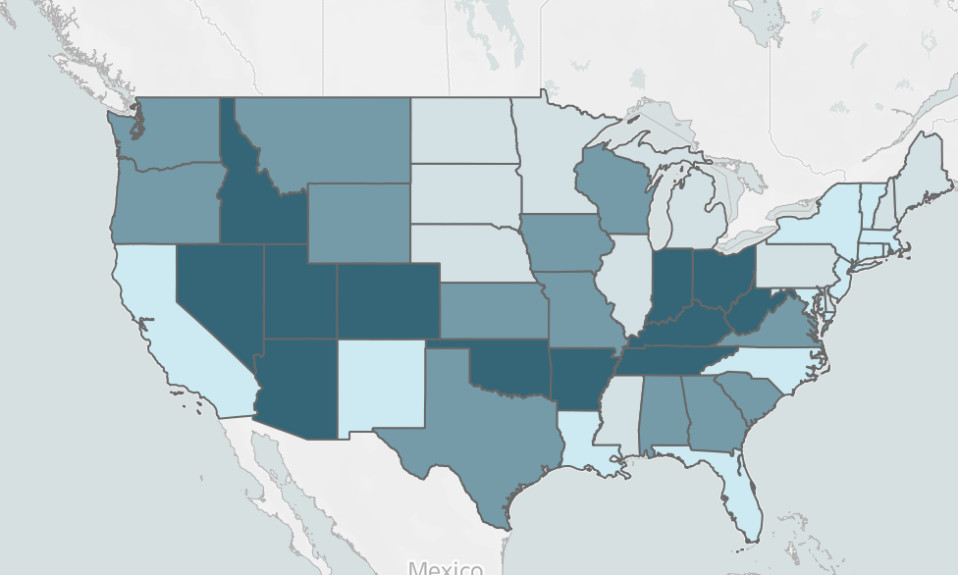
The nonprofit advocacy group Mental Health America’s (MHA) eighth-annual State of Mental Health in America Report ranks the 50 states and District of Columbia based on mental health and treatment access measures, while also highlighting pressing issues and recommending policy strategies to alleviate the growing public health problem.

In the 2022 State of Mental Health in America Report, MHA cites four goals of the report:
- To provide a snapshot of mental health status among youth and adults for policy and program planning, analysis and evaluation
- To track changes in the prevalence of mental health issues and access to mental health care
- To understand how changes in national data reflect the impact of legislation and policies
- To increase dialogue with and improve outcomes for individuals and families with mental health needs
MHA rates states based on a set of 15 mental health measures, separately ranking certain demographic categories and service issues (adults, youth, prevalence of mental illness, access to care) and tracking year-to-year changes in an effort to identify areas of need. It also notes the areas of biggest change from the previous MHA annual report.
[Mental Health America] speculates that the study likely underreports the current prevalence of mental illnesses in both children and adults.”
For example, in the adult rankings, the largest improvement identified from 2017 to 2018 was in Wisconsin’s move from No. 24 to No. 2 in percentage of adults with serious thoughts of suicide (a decrease of 5.17% to 4.66%). Meanwhile, in Hawaii the percentage of youth with a major depressive episode who did not receive mental health services increased from 56.2% to 71.0% during the same timeframe, representing a drop from No. 14 to No. 31 among all states. This information doesn’t speak to the effectiveness (or lack thereof) of any particular state program or policy, but it is in keeping with MHA’s goal of providing perspective and reinforcing that “data and information about disparities faced by individuals with mental health problems is a tool for change.”
Key Mental Health America Findings
The 2022 State of Mental Health in America Report includes data gathered through 2019, and MHA states that its findings “are most useful in providing some comparative baselines in the states for the needs and systems that were in place prior to the COVID-19 pandemic.” The organization speculates that the study likely underreports the current prevalence of mental illnesses in both children and adults.
Mental Health America says young people of color access depression care at a disproportionately lower rate than their white counterparts.”
Additionally, Mental Health America notes that one limitation of its latest report is the absence of information for people experiencing homelessness and who do not stay at shelters, people who are institutionalized (i.e., in jails or hospitals) and active-duty military personnel. Not surprisingly, MHA believes the overall numbers would be worse if data from those groups had been available.
With those caveats in mind, Mental Health America identified a handful of important data points in its 2022 report:
- In 2019, just prior to the COVID-19 pandemic, 19.86% of adults experienced a mental illness (nearly 50 million Americans).
- Suicidal ideation continues to increase among adults in the U.S., as 4.58% of adults reported serious thoughts of suicide—an increase amounting to 664,000 people from last year’s dataset (continuing an annual upward trend every year since 2011-2012).
- A growing percentage of youth in the U.S. live with major depression: 15.08% of youth experienced a major depressive episode in the past year (a 1.24% increase from the previous year’s dataset.)
- More than 2.5 million youth in the U.S. have severe depression, and multiracial youth are at greatest risk.
- More than half of adults with a mental illness do not receive treatment, totaling over 27 million people.
- The percentage of adults with a mental illness who report an unmet need for treatment has increased every year since 2011.
- More than 60% of youth with major depression do not receive any mental health treatment.
- Rates of substance use were increasing for youth and adults even prior to the COVID-19 pandemic: 0.07% for adults and 0.25% for youth over the previous year’s report.

Mental Health Spotlights
Mental Health America’s report features two spotlights, which the nonprofit describes as “a deeper dive” into its immediate policy priorities: (1) suicide prevention and access to crisis care, and (2) prevention and early intervention for children, youth and young adults:
Mental Health America cites a 2015 study that found people with untreated mental illnesses are 16 times more likely to be killed in a police encounter than other civilians.”
Suicidal Ideation and 988 Implementation addresses “the need for states to pass legislation to support a continuum of crisis services.” In addition to its own research on mental health and suicidal ideation, Mental Health America cites a 2015 study that found people with untreated mental illnesses are 16 times more likely to be killed in a police encounter than other civilians. The organization views the passage of the new 988 number for suicide prevention and mental health crises as an opportunity to begin building a continuum of crisis services—one that will prioritize equity, particularly for BIPOC individuals. By July 2022, all telecommunications companies will be required to make necessary changes to have 988 calls directed to the current National Suicide Prevention Lifeline call centers, although funding and implementation will be left to each state. MHA expects more resources to be needed in order to properly scale up the program.
Disparities in Mental Health Treatment for Youth of Color digs into the Substance Abuse and Mental Health Services Administration (SAMHSA) 2018–2019 National Survey on Drug Use and Health (NSDUH), analyzing disparities in the kinds of mental health care young people receive and where they receive it. Mental Health America says young people of color access depression care at a disproportionately lower rate than their white counterparts. Additionally, when students access mental health care at school, often it is because they don’t have access to specialty mental health services. MHA advocates for the long-term financial support of schools in this regard, including:
- Implementing comprehensive mental health education
- Increasing the number of mental health providers in schools
- Creating connections and coordinating with community-based mental health services
- Identifying processes and supports for screening and treating students
- Reducing the gap in care when students transition from high school to college and college to the workforce
Top photo: Joshua Rawson-Harris; bottom photo: Eric Ward