This “new” meth—based on previous versions of the drug—is even more dangerous, and has the treatment community flummoxed
By Jason Langendorf
Most Americans have had some level of exposure—whether through pop culture, the daily news or personal experience—to methamphetamine. But what many aren’t aware of is the clear line of distinction between the “old” version of the drug and P2P meth, a substance that seems to be quietly fueling a new public crisis of addiction, mental illness and homelessness.
While the opioid epidemic and skyrocketing opiate-involved overdose deaths make up the bulk of our current national discussion about drugs, addiction, treatment and prevention—and with good reason—only a fraction of that attention has been paid to the resurgence of methamphetamine as a substance causing harm across the country, including in regions and at rates previously not seen.
Meth has been available on a wide scale and has been in the public consciousness for decades. It isn’t a fashionable new party drug and hasn’t been reinvigorated by, say, innovation in its method of delivery. Yet both the data and boots-on-the-ground observations paint the picture of an unmistakable and insidious surge. What’s behind it? And compared to its predecessor, what makes P2P meth different—and so dangerous?
The Emergence of P2P Meth
The history of meth is an odd mosaic of chemists, World War II fighter pilots, long-haul truckers, college students on all-night crams, Hell’s Angels and Mexican cartels. When amphetamine, a widely used stimulant sometimes prescribed by physicians, was modified to create methamphetamine, the outcome was a synthetic offshoot featuring supercharged euphoric effects—and stronger adverse consequences.
The [manufacturing] method hadn’t been used in the past because it was low-yielding and produced a lesser product. But … manufacturers refined the technique and began finding new precursors—including dozens of chemicals like toiletries, solvents, tanning products and even racing fuel.
Manufactured almost exclusively using ephedrine and pseudoephedrine into the 2000s, meth began to draw more attention from the federal government and law enforcement. Brian Couey, director of outpatient services at the Betty Ford Center, notes that the crackdown took the same form as the approach to eradicating Quaaludes in the 1980s—precursor legislation. “The idea was, if we can restrict the precursors, then we can stop people from illicitly producing this,” Couey said in a recent P2P meth presentation. “And it was highly successful.”
When precursor legislation began making the availability of ephedrine and pseudoephedrine more difficult (and, in large enough quantities, even criminal), meth production was suppressed, supply was squeezed and the drug became more difficult and expensive to access. That, however, marked the dividing line between previous versions of the drug and P2P meth.
Government intervention led meth manufacturers to explore a previously little-used method of production: phenyl-2-propanone, which yielded two distinct components: a d-isomer (which produces the high experienced by the user) and l-isomer (which produces physical symptoms, such as an accelerated heart rate, as well as more toxic effects). The method hadn’t been used in the past because it was low-yielding and produced a lesser product. But with a new incentive to make it work, manufacturers refined the technique and began finding new precursors—including dozens of chemicals like toiletries, solvents, tanning products and even racing fuel.
From 2007 to 2010, the price of meth plummeted by 61% and purity increased by 114%. In 2010, the DEA reported that 69% of domestic meth samples collected by the agency were made using the P2P method. By 2012, that number had shot up to 96%. Within a few short years, what the public once knew as meth had been replaced by P2P.
Why Is P2P Meth Such a Threat?
How, precisely, is P2P more dangerous than its predecessors? Experts haven’t yet connected the dots. There is strong speculation that the toxic chemicals now being used as precursors by an increasingly disparate variety of producers in a Wild West of meth manufacturing are behind the current epidemic. What’s clear to anyone watching closely enough is that something has changed.
Whereas previous versions of meth produced feelings of euphoria, alertness and elevated mood, P2P seems to drive users toward isolation and neurological descent—paranoia, psychosis, delusions, hallucinations.
From 2015 to 2019, methamphetamine-involved overdose rates nearly tripled. According to Couey’s data, the Betty Ford Center found a 56% increase in treating patients diagnosed with a stimulant use disorder from 2018 to 2019, year over year. Clinicians, therapists, researchers, law enforcement—everyone recognizes the dramatic recent changes in the symptoms and behaviors of meth users.
Whereas previous versions of meth produced feelings of euphoria, alertness and elevated mood, P2P seems to drive users toward isolation and neurological descent—paranoia, psychosis, delusions, hallucinations—while precipitating more rapid physical deterioration.
As Chad Duncan, division director for Tennessee Adult Outpatient Addiction Services at Frontier Health, told the Kingsport (Tenn.) Times News: “The symptoms we see are way worse, the mental impairment is significantly worse, and its effects last longer. It’s really concerning.”
Previously, people who used meth were often able to hold down jobs, pay their bills, maintain a family and conduct their lives more or less without disruption. The toll of the ephedrine-based drug, by all accounts, wasn’t as great or swift as that of P2P. The psychological effects—what some have described, plainly, as “madness”—weren’t at the level of this new version. And because of P2P’s increased purity and accessibility, combined with its paltry cost, there seems to be no easy answer to untangling its harms.
“Meth is now so readily available. There’s an availability to it that is not the case with heroin or crack. It’s everywhere.”
—Matt Sharf, treatment center worker, to The Atlantic
“Meth reminds me of what alcoholics go through,” Matt Scharf, director of recovery programs at the Los Angeles-based treatment center Midnight Mission, told The Atlantic. “There’s alcohol everywhere. Meth is now so readily available. There’s an availability to it that is not the case with heroin or crack. It’s everywhere.”
The Ramifications
Where to start? P2P meth is increasingly being tied to growing homelessness, as well as rising harms within homeless communities, from giant tent cities in Los Angeles to teeming pods of people without shelter in Boston. And many experts claim that P2P is more difficult to treat because, in addition to there being no medication-assisted treatment (MAT) for meth, patients often aren’t stable enough for weeks (and even months) to accept help.
“When we do get people in treatment, we see that they do not always respond as well to standard mental health and substance use treatment approaches,” Duncan told the Times News. “This is likely due to the damage the meth has done to the brain.”
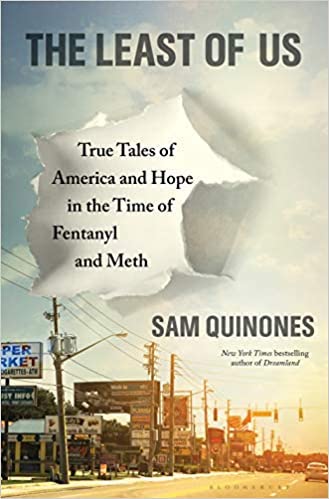
Sam Quinones, author of The Least of Us: True Tales of America and Hope in the Time of Fentanyl and Meth, recently told OBP that the narrative of P2P “is a supply story, pure and simple.”
Quinones, who lived 10 years in Mexico and has written two books on the country, says there needs to be an engagement between the U.S. and Mexico to squeeze the supply of P2P and its precursors. But cutting off the supply is only the first step. Quinones says the mental health symptoms must be treated and people housed before we ever will have hope of addressing the addiction.
“[I]t depends on the community, but certainly it might lead us to understand that there is no treatment—there is no housing of people until they are detoxed from this and until they have spent several weeks without this drug,” Quinones told OBP. “There’s no way of going forward with drug treatment until you can have people connected with other humans in some kind of real sense. And so that means first we need to rethink housing for the mentally ill and detoxing. I think that’s the very first step.”
Top photo: Shutterstock













