Medications designed to treat addiction to opioids and alcohol—and to reverse opioid overdoses—are saving and improving lives
By Jason Langendorf
The life-saving effects of medication-assisted treatment (MAT) are on full, dramatic display over the 39-minute run time of a nonprofit-funded 2017 documentary titled Heroin(e). The Oscar-nominated film follows three women—two public officials and a “street missionary”—as they take on the opioid epidemic in the town of Huntington, W.Va., where the overdose rate was reported at 10 times that of the national average.
Medication-assisted treatment is “the use of medications, in combination with counseling and behavioral therapies, to provide a ‘whole-patient’ approach to the treatment of substance use disorders.”—Substance Abuse and Mental Health Services Administration (SAMHSA)
In the doc, several harrowing scenes depict first responders administering NARCAN nasal spray—a brand name for the MAT drug naloxone—to unresponsive overdose victims, who, within moments of receiving the medication, are conscious and lucid. Clinically speaking, naloxone is a non-selective and competitive opioid antagonist that counters the potentially lethal decreased breathing that often results from opioid use. But the way it’s characterized most frequently—as the overdose-reversal drug—tells you all you really need to know about it, and why it’s so important in addiction treatment.
What Is Medication-Assisted Treatment?
Medication-assisted treatment is “the use of medications, in combination with counseling and behavioral therapies, to provide a ‘whole-patient’ approach to the treatment of substance use disorders,” as defined by the Substance Abuse and Mental Health Services Administration (SAMHSA). It is considered the “gold standard” of treatment, according to the National Institutes of Health (NIH).
Medication-assisted treatment saves lives, while increasing the chances a person will remain in treatment and learn the skills and build the networks necessary for long-term recovery.”—Michael Botticelli, former director, National Office of Drug Control Policy
But just as the word “assisted” is often glossed over in the understanding of MAT, so too is the “in combination with” qualifying phrase that makes up part of SAMHSA’s definition.
The term “medication-assisted treatment” was coined primarily to describe a pharmacotherapy for opioid use disorder (OUD), but it’s a concept that can be applied across addictions to alcohol, opioids and (soon, the hope is) possibly other substances.
Using exhaustively researched, Federal Drug Administration (FDA)-approved medications in conjunction with proven behavioral therapies that help people with addiction address related or underlying problems has been proven to be more effective than either treatment on its own.
“Medication-assisted treatment saves lives,” said former National Office of Drug Control Policy director Michael Botticelli, “while increasing the chances a person will remain in treatment and learn the skills and build the networks necessary for long-term recovery.”
MAT is a practical, compassionate and proven-effective tactic for treating people with addiction, helping them sustain recovery and prevent deadly overdoses.”
What Medication-Assisted Treatment Is Not
A common misconception about MAT goes something like this: It’s just swapping one drug problem for a different drug problem. As recently as 2017, in fact, a former U.S. secretary of Health and Human Services commented that “if we’re just substituting one opioid for another, we’re not moving the dial much” in America’s opioid crisis.
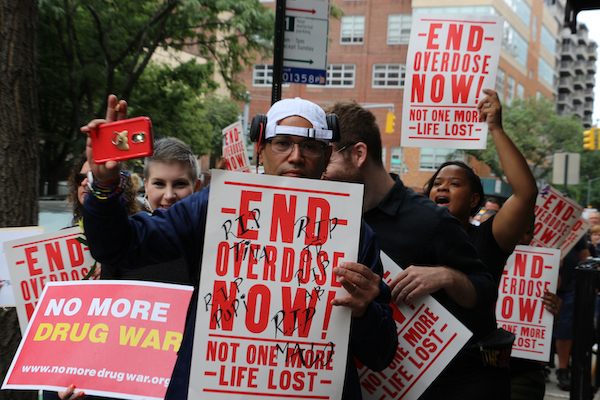
But the public’s understanding and perception of MAT has begun to change.
Medication is only a component of MAT as a form of addiction therapy. And although there are varying levels of risk involved with MAT drugs—including, in some cases, addiction—this is the case for most clinician-prescribed medications, administered for all sorts of conditions unrelated to addiction.
Additionally, by giving a person with addiction a safer and accessible alternative to street drugs, MAT helps reduce the incidence of HIV and hepatitis C. Reducing or ceasing drug use is a Herculean physiological challenge for many people, one that can prevent them from improving their health and life outcomes. MAT is a practical, compassionate and proven-effective tactic for treating people with addiction, helping them sustain recovery and prevent deadly overdoses.
Types of Medication-Assisted Treatment Drugs
There are many forms of MAT drugs, intended for a variety of disorders and purposes, and more continue to be developed. Most have the potential to cause mild to moderate side effects and come with warnings about interactions with other medications and substances. Be sure to consult a clinician before discontinuing use.
Below are some of the most commonly used MAT drugs:
MAT for both opioid and alcohol use disorder:
Naltrexone, sold under the brand names Vivitrol and Revia, blocks the euphoric effects associated with opioid and alcohol use, and helps people with addiction to reduce substance use and continue abstinence. Naltrexone is a non-opioid that does not have addictive properties. SAMHSA indicates “there is no abuse and diversion potential with naltrexone.”
MAT for opioid use disorder:
Buprenorphine (brand names: Belbuca, Probuphine, Buprenex, Butrans and Sublocade) curbs cravings and helps prevent other withdrawal symptoms for opioids. It comes in several forms—ranging from a tablet for dissolving under the tongue to a transdermal patch for intake through the skin—and is the first medication to treat OUD that can be prescribed and dispensed in a physician’s office, allowing for greater access to patients in need.
Methadone (brand names: Diskets, Methadone intensol and Methadose) reduces cravings and withdrawal symptoms by blocking or diminishing the effects of opioids. Taken daily in liquid, powder or diskette form, methadone can help patients sustain recovery and is safe when used as prescribed.
MAT for opioid overdose:
Naloxone (brand name: NARCAN), typically administered by first responders, is used to prevent opioid overdose, reversing the toxic effects of the OD. It comes in several forms, including intranasal spray (into the nose), intramuscular (into the muscle), subcutaneous (under the skin) and intravenous injection.
MAT for alcohol use disorder:
Acamprosate (brand name: Campral) helps people who are in recovery from alcohol use disorder (AUD) to avoid drinking. When used properly, acamprosate—a tablet taken three times daily—helps reduce the desire to drink alcohol. But it is not effective in preventing withdrawal symptoms after the user drinks.
Disulfiram (brand name: Antabuse) is typically used as a second-line treatment for people with AUD. The once-daily tablet creates a negative reaction to drinking by blocking the processing of alcohol in the body, causing side effects that may include nausea, headaches, vomiting and more as soon as 10 minutes after drinking. Disulfiram does not reduce cravings, however, and it has been largely replaced by acamprosate and naltrexone as preferred MAT therapies for AUD.
What the Future Holds for Medication-Assisted Treatment
MAT has become more widely accepted and thoroughly regulated only recently. For instance, federal law requires patients who receive medication through an opioid treatment pogram (OTP) to also undergo counseling.
As new medications are developed, stronger data reaffirms or reveals best practices for policy, and more attention and funding are directed toward America’s opioid crisis (and substance issues in general), MAT should be expected to become a more prominent part of the solution. The skepticism and stigma surrounding MAT have begun to lift, gradually, as programs across the country help to transform lives and communities.
MAT alone won’t end the drug epidemic, but it’s a vital component of an intelligent, compassionate and evolving approach to substance use disorder (SUD) treatment.
Photo: Sharon McCutcheon