The first psychedelics-inspired pharma to go public, MindMed is betting its therapies will revolutionize opioid addiction treatment
By William Wagner
September 2, 2020March 3, 2020, may well be remembered as a notable date in the annals of addiction treatment: It’s when MindMed, a Canadian neuro-pharmaceutical company, went public.
The IPO was significant for a couple reasons. For starters, MindMed became the first psychedelics-inspired pharmaceutical company ever to go public. More important, at least as cofounders JR Rahn and Stephen J. Hurst tell it, the stock offering provided an infusion of the resources MindMed will need to potentially change the face of addiction treatment, particularly where opioids are concerned.
The idea behind MindMed—behind an enterprise that is tapping the realm of psychedelics to treat addiction—isn’t nearly as far out as it might seem. Theories that certain psychedelic drugs have powerful anti-addictive qualities predate MindMed by several decades. Rahn and Hurst simply are taking the concept to the next level. They are deep into the process of developing 18-methoxycoronaridine (18-MC), a non-hallucinogenic medicine derived from the psychedelic substance ibogaine. That, however, is only the beginning. Their plan is to bring a series of similarly inspired therapies to market that address other maladies, such as PTSD and ADHD.
It’s been an amazing journey for MindMed, which came into existence in only 2019. The company’s lightning-speed growth can be traced in part to the chemistry between Rahn and Hurst. Rahn brings an entrepreneurial spirit to the mix; he’s a former Silicon Valley executive whose startups have included Upgraded Technologies, a company designed to help online users enhance their platforms. Hurst, meanwhile, is MindMed’s clinical point person, with more than 35 years of experience in the biopharmaceutical field.
TreatmentMagazine.com spoke with Rahn and Hurst about the origins of MindMed and the future of psychedelics-based therapies.

Q: What void in addiction treatment is MindMed seeking to fill?
Hurst: The advances in neuroscience over the past two decades have been pretty amazing. One of the things we’ve learned is that addiction is actually a brain disease. It doesn’t have anything to do with will. It’s a cooption of the reward-pleasure center in the midbrain, which is obviously an essential part of our survival instinct. It’s very primitive. The fundamental mechanism of reward and the neurotransmitters that drive the mechanism are pretty well understood. What we know is that the hallmark of addiction in the brain is the dysregulation of dopamine in this reward-pleasure center. With that in mind as you look at current approaches to addiction, it’s pretty easy to understand why they’re less effective than we’d like them to be. They actually aren’t treating the cause of the disease in the brain, which is this dysregulation of dopamine in the reward-pleasure center.
What you need to do is get in and affect neurotransmitter regulation as opposed to substituting something of less liability, like methadone for heroin or a nicotine patch for tobacco. Those are classic substitution therapies. Other approaches out there include aversion therapy, which is what Antabuse is. It makes one vomit when they ingest alcohol. The last one, which everyone knows these days because of the opioid crisis, is naloxone. It interrupts an opioid overdose by knocking the opioid off the opioid receptors in the brain.
Our [MindMed’s] approach to addiction is, why not treat the cause of the disease in the brain as opposed to using less effective substitution and aversion therapies or intervening at the point at which you’re providing a life-saving measure? [The driving force behind MindMed] is the brilliance of our founding scientist, Stan Glick. He’s one of the most underappreciated scientists in the world, in my opinion. I’ve been working with him for more than a decade now.
Q: What’s the theory behind psychedelics-based addiction treatment? How does it work?
Hurst: The origins of the story go back to the late 1950s, early 1960s. There was a [scientific researcher] by the name of Howard Lotsof who was a heroin addict. He got in with the Timothy Leary crowd at the time, and they started trying everything in the world that was associated with psychedelic behavior. There’s a drug called ibogaine that is derived from a shrub in West Africa and is a very potent hallucinogenic. Howard and his colleagues were heroin addicts, and they basically went out and took heroic doses of ibogaine. They did not use heroin [during the trips], and they did not have withdrawal after they came off the trips. Howard declared this a cure for addiction, believing full well that the full hallucinogenic experience was essential. He went around for the next decade or more promoting ibogaine as anti-addictive.
Eventually, Howard found his way to Stan Glick, a neuropharmacologist at Albany Medical College. Stan was interested in addiction, and he was convinced by Howard to try ibogaine. What Stan found really intriguing in the animal self-administration models he did was that long after the effects of ibogaine wore off, there was still attenuation of the self-administration of addictive substances by the animals. This suggested to Stan that the anti-addictive properties of ibogaine might, in fact, be independent of the hallucinogenic or psychedelic properties of ibogaine.
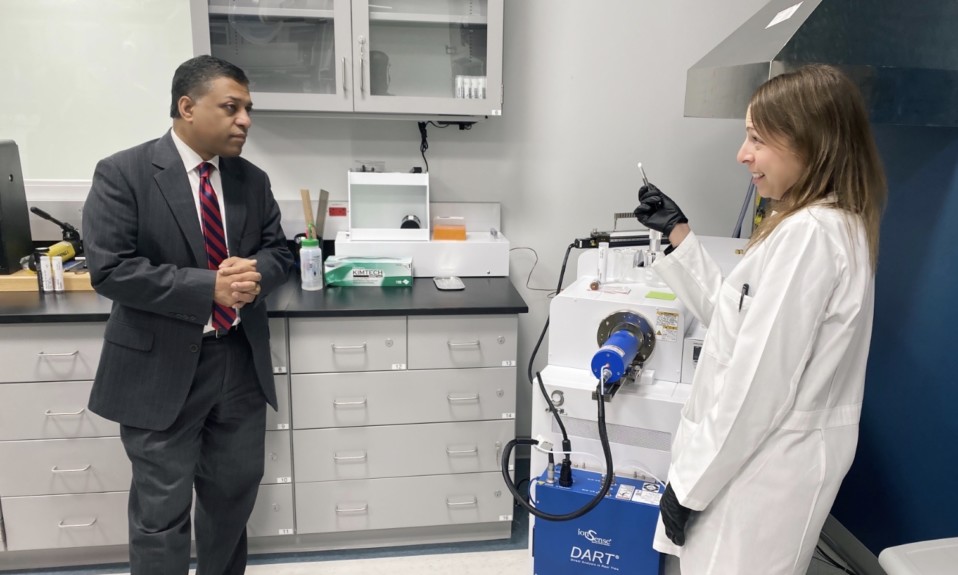
He collaborated with a chemist at the University of Vermont, and they synthesized a bunch of analog molecules to the backbone molecule of ibogaine. They started testing those to see which ones had anti-addictive properties, and then they would see if they had any suggestion of hallucinogenic properties. Equally important with ibogaine is it can induce fatal cardiac arrhythmia. The 15th one they screened is what we’re now in the clinic with, which is 18-MC. It’s a completely synthetic molecule. There is no evidence in humans or animals that it retains any hallucinogenic properties or has any cardiovascular safety issues. It is a far superior alternative to ibogaine as an addiction treatment.
Our [MindMed’s] approach to addiction is, why not treat the cause of the disease in the brain as opposed to using less effective substitution and aversion therapies or intervening at the point at which you’re providing a life-saving measure?”—Stephen Hurst, cofounder of MindMed
Q: What drew you two to this venture?
Rahn: Steve and I met through a professor at NYU. We both saw the potential for psychedelics as medicines. What we ultimately concluded was that there needed to be a company that could bring some of these medicines forward. Steve had a long background of developing medicines. In addition, he had spent quite a lot of time advising the nonprofits in the psychedelics arena on how to design drug trials. We met in New York, and that was the beginning of MindMed. It’s moved quick.
The reason I personally got involved in the space is I saw that addiction and mental health were growing problems in America. There hadn’t been any innovative or disruptive solutions to these problems. I thought psychedelics had potential, but I didn’t necessarily see them being pushed forward by a company in the addiction space. If you look at what Steve has been able to do with 18-MC, it’s very interesting. It almost lowers the bar for a lot of addiction therapists. It’s focused on, “How do we actually treat patients and not put them on a pill a day for the rest of their lives?”
Q: You two have different backgrounds. What is it about your chemistry that has enabled MindMed to come so far in such a short period of time?
Hurst: [laughing] It’s called a healthy tension.
Rahn: I think the reality is we both have skill sets that are complementary. I had never developed drugs before starting this company. I had started companies, but I think what we’re doing is developing a brand new space. This has never been done. I view the company as a pioneer in psychedelic-inspired medicine. We’re focused on addiction, but we’re doing some groundbreaking things [in a number of areas]. With Steve’s experience and knowledge around psychedelics and my experience in raising capital getting the right folks behind us, I think we’re going to be very successful.
Q: At first glance to a layperson, there would have to be a certain amount skepticism about psychedelics-inspired treatments for addiction. How do you overcome that?
Rahn: Before Steve answers—because he has a really good response—I just want to give you a little secret and fact. You know what the 13th step of AA was supposed to be? An LSD trip.
Hurst: Bill Wilson, the founder of Alcoholics Anonymous, was overruled by this board. But let me answer your question really directly. One of the things you and your colleagues in the media can do is help us to educate people and dispel the myths. Let’s go after the first myth: that LSD is addictive. It is a very, very potent modulator of neurotransmitter activity in the brain. This is true of essentially all traditional hallucinogens. These are not what are known as “reinforcing compounds.” You do not go through withdrawal when you stop using them; you do not crave them. You might think it would be nice to have that trip over the weekend, but the cravings—
Q: It’s not like a cigarette, for instance.
Hurst: No, it’s not like a cigarette. Hallucinogens do not exploit the reward mechanism in the brain. It is a different neurotransmitter that is being affected. We have to go after the myths and beliefs people hold about psychedelic compounds. As Albert Hofmann recognized when he invented LSD, the opportunity to use these agents in a therapeutic manner is tremendous. That is where we see these compounds going. From what we can see, the anti-addictive properties don’t have much of anything to do with the hallucinogenic aspect of it. Their potential in PTSD, chronic depression, ADHD and anxiety disorders is unparalleled by anything that exists in pharmacopeia. There’s nothing that can approach what these drugs have in terms of potential.
Q: To what do you attribute MindMed’s rapid growth?
Rahn: I’ll summarize quite quickly: These are really big health problems that we’re solving in America. For addiction, anxiety and mental health in general, there aren’t great solutions on the market. The reason for the growth [of MindMed], I believe, is these things need to get to market. Obviously, we have to do the clinical trials, but America needed this stuff yesterday.
Q: In March, you became the first psychedelics-based pharmaceutical company to go public. What was the thought process behind taking MindMed public?
Rahn: Drug development is not cheap. We understood that we needed to build a platform that wasn’t going to develop just one medicine but multiple medicines. In order to do that, you need to be a public company, because you can attract a shareholder base that is vast. You can also attract retail investors. That was always the strategy.
Q: What do you see as the future of psychedelics-based treatments?
Hurst: We saw a pretty significant market initially, just by the fact that addiction alone is the world’s biggest unmet medical need. When you add mental health to that, you end up with a vast patient population that is being underserved by current approaches. We just hope we can get our medications through and approved in a manner that ends up doing a lot of good for people.
Photo: David Clode