Epidemic is symptom of systemic methamphetamine problem
By Jason Langendorf
Findings from a series of recent, unrelated studies confirm a steep rise in the use of methamphetamines in the United States, fueling concerns about the next drug epidemic, however treatment is within reach.
The American Medical Association reported a 245% increase in meth-related hospitalizations between 2008 and 2015 (during a period when opioid-related hospitalizations rose only 46%) in a 2019 study. In January, U.S. News & World Report cited a study of more than 1 million urine tests (administered mostly by clinics dealing in primary care, pain management, and substance disorder treatment) that returned positive for meth use, up from 1.4% in 2013 to 8.4% in 2019.
Historically, often times after there’s been an epidemic of opiate use, it’s been followed by a big problem with stimulants. We saw it in the ’70s with heroin and then cocaine in the ‘80s. And of course now we have a huge opioid problem in this country.”— Christopher Yadron, PhD, LCPC, CADC, Hazelden Betty Ford Foundation regional vice president of the West and administrator of the Betty Ford Center
“The most important data, the most factual data, says the number of methamphetamine-induced toxicities, ER visits, and overdoses are increasing,” says Dr. Paul Earley, MD, DFASAM, president of the American Society of Addiction Medicine. “And the overdoses with other substances, more of those are showing up with methamphetamine present in the blood at the same time.”
Why Is Methamphetamine Use Increasing?
Treatment experts have noticed the rise, anecdotally, or in data analysis, but now there is hard evidence indicating methamphetamine use is skyrocketing. There also seems to be consensus about the factors associated with the drug’s newfound popularity—what Dr. Earley notably refers to as a “pendulum” effect.
Christopher Yadron, Ph.D., LCPC, CADC, is Hazelden Betty Ford Foundation’s regional vice president of the West and administrator of the Betty Ford Center in Rancho Mirage, Calif. Speaking on a Hazelden Betty Ford-produced podcast last June, Yadron explained the rise in methamphetamine use.
“I think drug trends shift for a variety of reasons, whether it’s a perception of harm, access, cost. One of the things that we’ve seen, if you look, historically, oftentimes after there’s been an epidemic of opiate use, it’s been followed by a big problem with stimulants. We saw it in the ’70s with heroin and then cocaine in the ‘80s. And of course, now we have a huge opioid problem in this country. But over the last several years, crystal meth has once again become a huge problem for us.”
Dr. Earley saw this effect as far back as the 1980s, in the habits and perceptions of the patients admitted to the Atlanta treatment clinic he ran early in his career.
The people who have discontinued methamphetamine have higher difficulties with impulsivity than other people and have problems processing data in a logical fashion, which you really have to do for self-care skills for recovery … It makes it a more difficult subset of the addiction problem to treat.”—Paul Earley, MD, DFASAM, president of the American Society of Addiction Medicine.
“But It’s Not Heroin”
“People were coming in [who had been] using cocaine and smoking crack, and they would say, ‘Well, doc, it’s not heroin or anything.’ And I would say, ‘I understand, but you are really in trouble with this.’ And then as the cocaine epidemic waned, up comes the heroin epidemic,” he says. “And now people are coming in and saying about cocaine, ‘Well, it’s not heroin or anything.’ This is just part of the zeitgeist—the public perception of safety—and the one that’s touted the most as being dangerous is the one that people avoid. So inevitably, for those who aren’t suffering from addiction to one of the drugs, they’ll start switching.
“The first time someone said it,” Earley recalls, “it kind of smacked me upside the head. I thought: ‘Oh my goodness, this is the problem—people are confusing addiction with a quality that occurs in drugs and not something that’s wrong with their brain.’”
Legislation and oversight of certain over-the-counter substances in the mid-2000s made it more difficult in the United States to buy the necessary ingredients to make crystal meth. The result was a leveling off of methamphetamine use—and the onset of the opioid epidemic that captured so much of the country’s attention since then. Today, with methamphetamine use again spiking— and in light of an alarming long-term increase in accidental overdoses involving any drug—experts such as Earley stress the importance of understanding the current crisis not as one surrounding a single insidious drug, but as the symptom of a larger systemic problem.
“If people have trouble with one substance, an addiction or substance use disorder, they’ll switch to another one—to another drug,” Earley says. “That’s just part of the illness. It’s shortsighted of us as a society to talk about the drug problem being a problem with a specific drug because it invites this pendulum.
A Brain, Not Addiction, Problem
“Addiction is a problem with the brain, not a quality of a specific substance. Human beings are going to always have addiction disorders as long as there are medications which cause an abnormal response to those medications.”
Earley admits, however, the presence of unique challenges in the treatment of methamphetamines addiction and treatment.
“Methamphetamines like cocaine produce a near-psychotic state and can increase violence,” Earley says. “The heroin-addicted individual tends to be, if anything, more on the quiet, introverted, peaceful side, if you will. Even in withdrawal, they’re agitated but not dangerous. [That’s] versus methamphetamines and cocaine, which can induce violence in a toxic state, which is really problematic.
“Even if it’s not dangerous to external people, the people who have discontinued methamphetamine have higher difficulties with impulsivity than other people and have problems processing data in a logical fashion, which you really have to do for self-care skills for recovery. You have to figure out how to get to a meeting, you have to figure out how to make decisions that are going to keep you away from your using friends. All those things are more difficult for methamphetamine users. And in some ways, it makes it a more difficult subset of the addiction problem to treat.”
Medication Assisted Treatment
Another frustration is the lack of proven medication assisted treatment (MAT) for methamphetamine addiction. The panic surrounding the latest wave of opioid addiction helped rally support and spur research that led to the proliferation of treatment medications such as methadone, buprenorphine and injectable naltrexone. Earley points to “a lot of research going on that may help the treatment” of meth addiction in the future. But he and other experts continue to caution against hopes for a magic bullet, whether in the treatment of methamphetamine use disorder or any other form of addiction care.
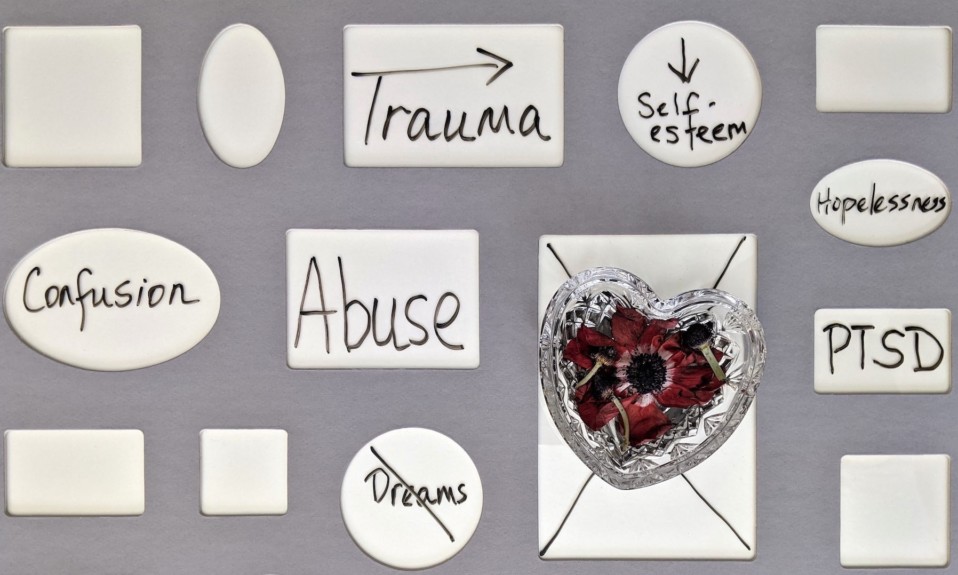
Says Yadron: “We’re still treating people, human beings who are suffering from substance use disorders. Like any drug of choice, it ends up leading people to a life of alienation, isolation, disconnection from themselves, from others from their higher power.”
Individuals suffering from meth addiction aren’t without hope. But it’s important that anyone seeking help, for themselves or a loved one, understand treatment as a continuum of care—an ongoing, holistic program that isn’t a one-size-fits-all solution.
People are confusing addiction with a quality that occurs in drugs and not something that’s wrong with their brain.—Dr. Paul Earley
“The proper care of addiction requires a multidisciplinary approach,” Earley says, “with people from various educational and experience backgrounds as care providers, so that we can maximize the recovery and remission from addiction illnesses.”
Photo: Abigail Keenan