Plus: A smartphone app that helps pregnant women quit smoking, and the effect of early pharmacological treatments on substance use
By Mark Mravic
Screening methods to identify potential alcohol misuse can be problematic, often relying on self-reports and interviews that may contain biases. Could social media serve as a public resource to help identify problem drinkers and issues around alcohol misuse? A new study looked at Facebook to find out.
Also this week, research into the effectiveness of financial incentives delivered through a smartphone app for pregnant women to quit smoking, and treating childhood mental illness with meds early to prevent later substance use.
From Alcoholism: Clinical and Experimental Research:
Facebook Users’ Language Can Identify Risk of Hazardous Drinking
Social media has become an increasingly useful tool to explore issues in substance use and addiction. Previously we reported on studies that looked at Reddit posts to identify the emergence of designer drugs and explore the notion of self-harm as addiction. Now researchers from the University of Pennsylvania and Stony Brook University have analyzed Facebook posts to identify those at risk of dangerous drinking.
The researchers collected data from 3,664 Facebook users who consented to participate in the study. Based on users’ self-reported alcohol consumption, the population was divided into low-risk (73%) and high-risk (27%) drinkers. An artificial intelligence application called “contextual embeddings” that interprets language in context then analyzed the users’ posts. The study found that the AI app was 75% accurate in identifying high- and low-risk drinkers based on the language in their Facebook posts, a success rate that the researchers say is higher than traditional models used to spot problem drinkers and those susceptible to alcoholism.
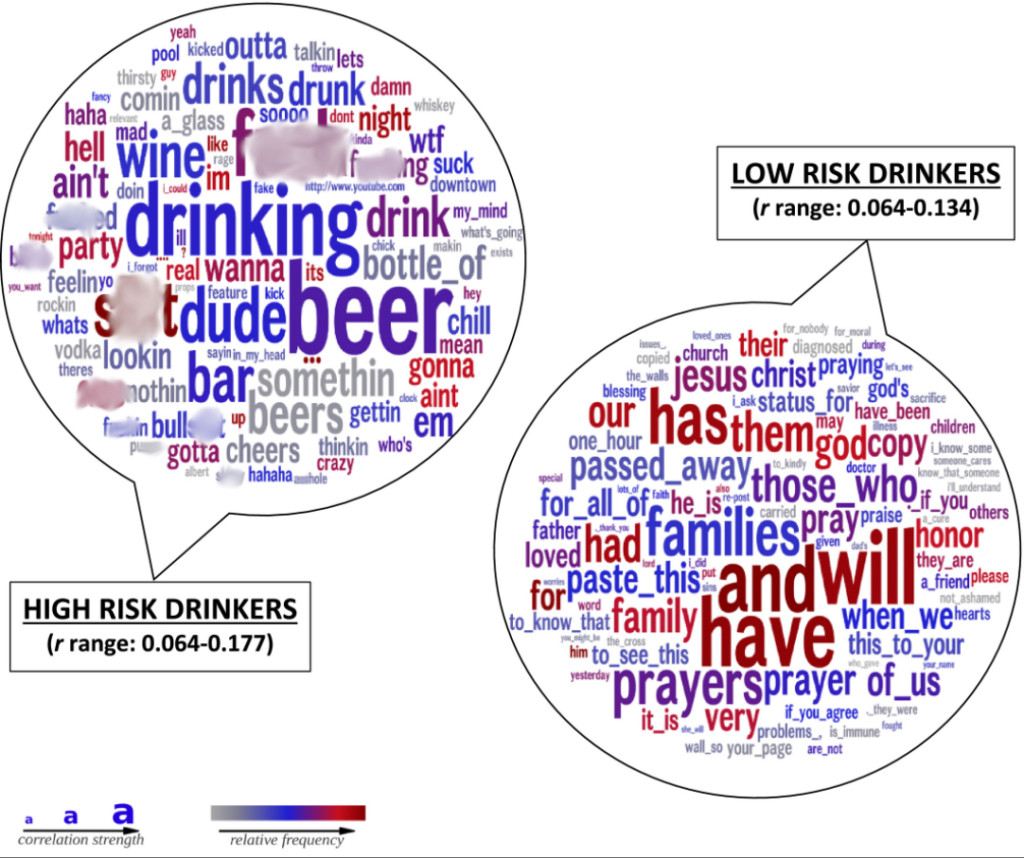
Words and phrases that the researchers said were predictors of heavy drinking include those related to partying; those involving swearing; informal language such as dropping the final “g” in words; slang and internet shorthand; and negative emotions. Language associated with low-risk drinking included faith-based and relationship terms, and future-oriented references.
Researchers suggest high-risk language may reflect impulsivity and sensation-seeking in the users, as well as easier access to places to drink, factors that can lead to heavier drinking. The low-risk language may correspond to broader support networks and a brighter personal outlook, tending to moderate alcohol consumption.
“What people write on social media and online offers a window into psychological mechanisms that are difficult to capture in research or medicine otherwise,” said co-author H. Andrew Schwartz, PhD, of Stony Brook, in a release. The authors concluded, “Social media data serves as a readily available, rich and under-tapped resource to understand important public health problems, including excessive alcohol use.”
From JAMA Network:
Paying Pregnant Smokers to Quit—Through Their Phones
Data shows that smoking during pregnancy is the leading preventable cause of poor pregnancy outcomes in the U.S. The solution: Pay women to quit. Contingency management (CM)—in which subjects receive a reward for abstinence behavior—has been shown to be an effective way (some say the most effective way) to get pregnant women to stop smoking. But CM programs for smoking cessation typically have required in-person clinic visits, limiting their reach and effectiveness. To address the issue, researchers at the University of Vermont—a pioneer in smoking-cessation programs for pregnant women, in a highly rural region with limited public transportation—looked at whether a smartphone app for CM could achieve similar results.
Women in the financial incentive group were more than four times as likely to quit smoking as the control group.
In the study, involving 90 pregnant women across the country, one group followed typical best practices for smoking cessation, comprising brief counseling and referral to a telephone quit line, while the other underwent best practices plus the smartphone intervention—which included digital monitoring of smoking behavior and the delivery of financial incentives through an app from Dynamicare Health. Participants videoed themselves taking saliva tests for nicotine and received notification of the results through the app. When samples showed they hadn’t been smoking, money was added to a debit card they’d received at the start of the study. The interventions lasted from pregnancy through the first 12 weeks postpartum, with rewards escalating for each consecutive smoke-free test. Maximum potential earnings were about $1,620; mean earnings in the study were $331.
The study found that women in the financial incentive group were more than four times as likely to quit smoking as the control group, across both the pregnancy and postpartum periods (though abstinence among both groups decreased over time after giving birth). As previous research has pointed to significant cost-benefits to such programs, with each dollar invested shown to yield between $4 and $12 in economic benefits, researchers say the smartphone app underscores the potential to expand such cost-effective treatment to a wider swath of the population, including “those with socioeconomic disadvantage, rural residents, Indigenous individuals, and other racial and ethnic minority individuals.”
From the Journal of Child and Adolescent Pharmacology:
Early Pharmaceutical Treatment Can Reduce Later Substance Use Disorders
How important is early childhood intervention for mental illness in preventing later addiction? Researchers out of Massachusetts General Hospital examined 26 long-term studies involving nearly 6 million children and adolescents with ADHD, major depressive disorder and psychotic disorders, and found that pharmacological treatments for pediatric psychiatric problems appeared to reduce the development of later substance use disorders (SUD) by 30% to 35%. The results were more notable when treatment was initiated early and for longer periods.
“We need to identify and treat psychiatric disorders early in life.”
—Timothy Wilens, Massachusetts General Hospital
“The fact that the literature shows that juvenile-onset psychiatric disorders are significant risk factors for SUD coupled with our findings that medication treatment reduces that risk affirms that we need to identify and treat psychiatric disorders early in life,” said Timothy Wilens, MD, who led the research team. “Picking it up early and treating these kids as long as they require treatment leads to a much better outcome when it comes to substance use disorders.”
Top photo: Fred Moon; word cloud image: Rupa Jose and Andrew Schwartz