The Georgia addiction treatment facility’s name change signals new offerings, yet its mantra—“Everyone deserves the highest-quality care”—remains the same
By Jennifer Taylor
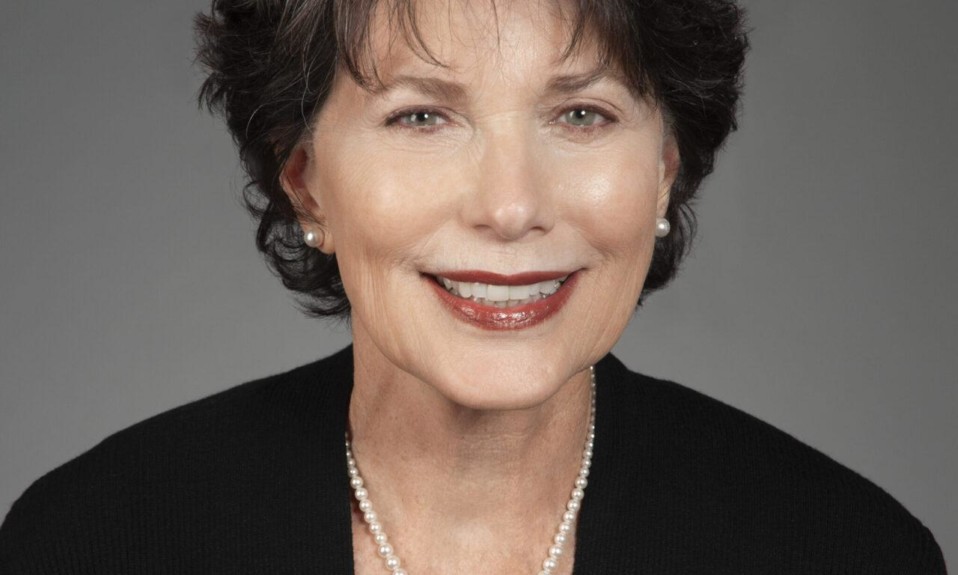
January 21, 2021Thirty-one years ago, Ascensa’s Suzanne Shaffer had no idea what she was getting into when she accepted a job at the then-St. Jude’s House, an Atlanta-based halfway house for men, specifically repeat court offenders recovering from alcohol use disorder (AUD).
It was 1989. Shaffer was a recent college graduate and the country was in the grip of a crack cocaine epidemic. “I started out by doing whatever was needed,” she says. “The agency was small, and I was given an opportunity to learn and grow.
“And I never left.”
Three decades later, Suzanne Shaffer, M.S., now leads the center, rebranded in 2020 as Ascensa Health. Named president and CEO in 2012, Shaffer has held almost every job possible in the treatment facility, working initially as a volunteer coordinator and then in case management. She later stepped into roles touching nearly all aspects of the center, including director of development, grant writer, fund-raiser, director of administrative services and chief operating officer. Her day-to-day responsibilities have included the operations of human resources, facility management and food service.
These are people that we can’t afford to lose to the disease of addiction. I believe treatment works. People recover and they are valuable people. They are somebody’s child, they are somebody’s brother. They’re important.”—Suzanne Shaffer, President and CEO, Ascensa Health
As Shaffer’s professional development evolved, so too did the organization. Last year, the center rebranded itself as Ascensa Health from St. Jude’s Recovery to help distinguish the center from the similarly named St. Jude Children’s Research Hospital in Memphis, Tenn. The name change also signaled the growth at the federal- and state-funded center since its founding in 1962, and reflected the broadening of its services and vision for the future.
What remains the same: Ascensa’s foundational mission to treat uninsured people with substance use disorder, regardless of their ability to pay.
Ascensa Health’s Approach to Recovery
Ascensa Health at St. Jude’s Recovery Center owns eight facilities in the metro-Atlanta area and provides services based on “the belief that addiction is a disease and that treatment must focus on the whole person.”
Ascensa applies evidence-based approaches that address substance use and mental and physical health. The full scope of programs and services include residential detoxification, residential and outpatient treatment services, medication assisted treatment (MAT), recovery residences, intake and assessments, treatment planning, addiction and co-occurring mental health treatment, life-skills training, employment services, health services, nutrition education, individual and group counseling, 12-step education and groups, family services, parenting education, and continuing care.
“These are people that we can’t afford to lose to the disease of addiction. I believe treatment works. People recover and they are valuable people. They are somebody’s child, they are somebody’s brother. They’re important,” Shaffer says.
Shaffer recently spoke to TreatmentMagazine.com about Ascensa Health’s dedication to the people it serves and how the organization is impacting the treatment field.

Q: To what do you attribute Ascensa’s unique success in treating addiction?
A: One of our greatest strengths is our ability to adapt to the changing needs in the community, and in the individuals we serve. Nearly 60 years ago, it was a halfway house for men with chronic alcoholism. As the years went by, the drug of choice changed. We’ve expanded throughout the years to serve both men and women. In 2004, we purchased a school building that is now our Family Care Center. This program actually broke through a daunting barrier for women seeking treatment because the center houses children, too. It is currently housing 22 women, who can bring up to three of their dependent children with them while they’re in treatment. It offers them the ability to get and stay in treatment and keep their children or be reunited with them following their care.
Q: What is your treatment mission for the Family Care Center?
A: The greatest barrier for women receiving treatment is that they are the primary caregivers for their children. The Family Care Center program removes that barrier by allowing their children to come into treatment with the mothers. As with all the programs, we provide a treatment model that is person-centered and evidence-based. Some of the modalities that we use include CBT, DBT, the Matrix Model, mindful meditation, yoga and psycho-educational groups that include relapse prevention, anger management and the 12-step self-help model.
We also provide programming that is specific to this population, including trauma recovery and the empowerment model, therapeutic childcare, parenting education, bonding, case management for those working with DFCS, and parent/child therapeutic activities. Providing support for mothers with their children allows our clients to not only receive treatment services, but it also adequately prepares them for long-term recovery as working, self-sufficient parents in recovery.

Q: What is Ascensa working on innovating?
A: We are addressing recidivism in the criminal justice system. That’s what we’ve been working on for a couple years. We’ve always had a population that is coming from the courts, criminal justice system. One of the barriers people face coming out of the prison system is continued treatment for their substance use. Without continued support, these individuals are likely to begin to use and again, falling back into the same pattern that landed them in the criminal justice system to begin with.
We’re currently partnering with state and county criminal justice systems to provide outpatient services together in the community. We’re providing additional support so that we promote the same recovery and reduce the chances of recidivism, which has an enormous impact on the individual and the community.
Georgia was fortunate to have former Gov. Nathan Deal pass several initiatives to deter crime rather than punish it, including the creation of Georgia’s accountability courts. Funding went to more accountability courts so individuals were referred to treatment rather than jail. Accountability courts provide alternative sentences to help inmates with substance abuse and mental health issues.
We’re the place where you go when you can’t go anywhere else. Because if you’re uninsured, you can’t get in treatment. This is why I love it here.”—Suzanne Shaffer
Q: How are you tracking your success?
A: For us, that means a client leaves with the tools they need to maintain their recovery, become employed, [and] transition to a permanent housing environment that’s conducive to their recovery process—we consider that a success.
Currently, our performance measure and management program tracks client progress from beginning to end. We take into account a number of factors that include improved functioning, improved health status, improved income, length of stay. An important one for us, because they were homeless or uninsured prior to coming here, we want [our clients] to move to permanent housing.
We analyze all this information monthly, quarterly and annually to identify any trends early on and take action to improve them.

Q: What do you wish you could change about the treatment field?
A: I still think the field needs to focus on more education to reduce the stigma of substance use disorder. There’s been great strides made for mental illness, but we still struggle with acceptance that addiction is a brain disease. Many people don’t receive the help they need because of the stigma attached to substance use. What many fail to see is that substance use is tightly connected with mental illness.
This year, nearly 60% of our clients have both a substance use and a mental health disorder. They go hand in hand, but the stigma that continues around substance use is still a barrier for those who need help.
The reality is that substance use disorder is a disease. Substance use is tied to mental health, and substance use is treatable. Nobody blames a person for getting cancer or someone with asthma for having asthma. You wouldn’t say they are cancer or they are asthma; they have cancer, they have asthma.
But we do call someone with an addiction an addict. That’s the stigma.
This year, nearly 60% of our clients have both a substance use and a mental health disorder. They go hand in hand, but the stigma that continues around substance use is still a barrier for those who need help.”—Suzanne Shaffer
Q: After 31 years—and more to come—in this field, what is your TTT: top treatment takeaway?
A: It’s something really simple. I really believe treatment works. And I believe people can and do recover. It’s hard. Addiction isn’t pretty. I just believe in hope.
I always hope that people choose recovery. I believe their lives can be restored. I really do. And I don’t know if that’s profound or just plain simple.