Plus: Lapses by weed dispensaries in California and the quest to find out what nonfatal ODs to do the brain
By William Wagner
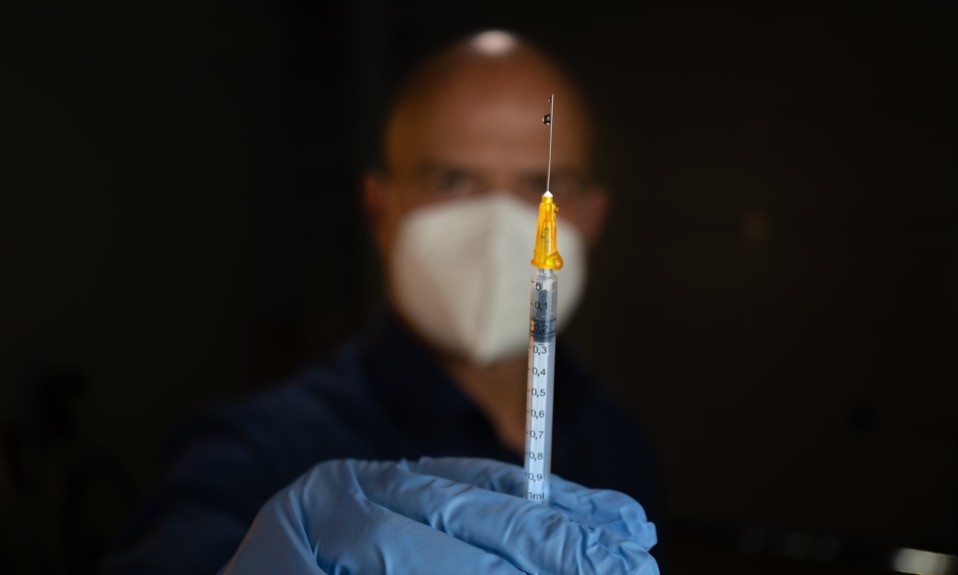
What if there were an opioid vaccine? It would be a game changer—and it’s not some distant dream. One is being tested right now at Columbia University.
We also look at California weed dispensaries and their lax screening of minors, and an attempt by researchers from West Virginia University to determine the damage a nonfatal overdose inflicts on the brain.
From Columbia University:
A Cure for Opioid Addiction?
In the battle against opioid addiction, scientists from the Columbia University Vagelos College of Physicians and Surgeons are attempting to deal a decisive blow. They’re working on an opioid vaccine that is in a phase 1a/1b clinical trial—in other words, the relatively early stages of testing. If the vaccine works, it could go a long way in ending the opioid epidemic, which has claimed hundreds of thousands of lives.
“We have good medications to treat opioid use disorder, but about half of the people who use these medications relapse after about six months,” Sandra Comer, Ph.D., a professor of neurobiology in the Vagelos College of Physicians and Surgeons and the principal investigator of the trial, said in a news release. “A vaccine that lasts for several months, given in combination with any of these medications, could help many more people beat their addiction and potentially protect them from an overdose death if a patient relapses.”
The opioid vaccine was originally developed by Marco Pravetoni, Ph.D., a professor of pharmacology and medicine at the University of Minnesota Medical School. It works by generating antibodies to oxycodone, a prescription opioid that has been one of the roots of the opioid crisis. In essence, the vaccine is designed to prevent oxycodone from getting to the brain and triggering an overdose.
Similarly designed vaccines could counter two other particularly deadly opioids, heroin and fentanyl. “Clinicians would be able to give the oxycodone vaccine to individuals who mainly use that particular drug but could also administer additional opioid vaccines for those who use other opioids or to prevent patients from switching to another opioid,” Comer said.
From JAMA Pediatrics:
California Dispensary Screening Falls Short
When it comes to keeping minors away, California dispensaries aren’t getting the job done. So say University of Southern California researchers, who studied 700 licensed cannabis dispensaries in the state.
As more states legalize cannabis, we need better mechanisms, including funding and agency authority for random compliance checks, to ensure that regulations are being followed—just as we did with tobacco.”—Rosalie Liccardo Pacula, University of Southern California
“Our data shows that youth can potentially be exposed to cannabis marketing and products despite California appearing to have tight laws,” Rosalie Liccardo Pacula, Ph.D., one of the study’s authors, said in a news release. “As more states legalize cannabis, we need better mechanisms, including funding and agency authority for random compliance checks, to ensure that regulations are being followed—just as we did with tobacco.”
From Drug and Alcohol Dependence:
What About Nonfatal Opioid ODs?
We’re still not exactly sure, despite the best efforts of a research team from West Virginia University. Since only 4 to 18% of opioid overdoses that are treated in a hospital or pre-hospital setting result in death, the ones that don’t kill you are important to study. The West Virginia University researchers sought to find out what nonfatal overdoses do to the brain. While they are relatively confident an overdose can cause some manner of cognitive impairment, their findings were inconclusive.
As the team writes in Drug and Alcohol Dependence, “Respiratory depression is a defining characteristic of opioid overdose and prolonged cerebral hypoxia may cause brain injuries and/or neurocognitive impairments. The onset, characteristics, and duration of such injuries is variable and additional research is needed to understand their clinical implications.”
Photo: Mika Baumeister