With no physical beds or walls, this nature-focused treatment center specializes in guiding teens and young adults along the trail of recovery
By Jennifer Taylor
October 29, 2020Situated on the southern border of Utah just north of the Arizona stateline, the scenic American West town of Kanab lures seekers of all kinds with its Navajo sandstone cliffs and canyon in captivating hues of red, orange and yellow.
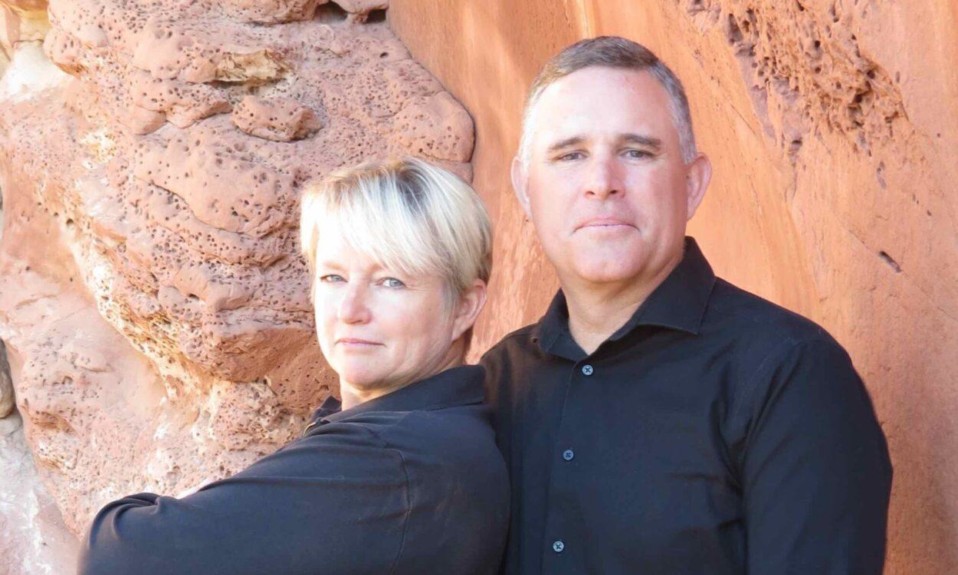
That pull and the healing power of the desert is what Shayne Gallagher, cofounder and executive director of WinGate Wilderness Therapy, and his team of specialists, including his wife, cofounder and director of operations Sheri Gallagher, cite as the source for their programs. They serve teens and young adults who struggle with alcohol and drug addiction, behavioral disorders and a range of mental health issues.

WinGate Wilderness Therapy, nearing its 13th year, is an alliance-based, experiential treatment approach that relies on connection, trust, respect and agency to inspire change in individuals. One of its biggest challenges from an insurance perspective, according to Gallagher, is the lack of physical walls and beds. Instead, WinGate begins its participants’ recovery and care journeys on the trails where hiking and camping are intertwined with therapy and self-discovery.
From the participants’ point of view, one of the biggest challenges—and benefits—is the treatment environment itself. It’s in the middle of nowhere. This lack of distraction in the desert is what Shayne Gallagher points to as part of WinGate’s formula for success.
Q: How did you first get into the addiction treatment field?
A: In 1990, through a series of events, I found out about wilderness survival. They didn’t call it wilderness therapy yet, but it was a new industry working with addicted kids and mentally, emotionally, behaviorally compromised children. I worked my first training week and thought that this was the most asinine job anybody could have to work with a bunch of teenagers. There was just no way I was going to do it, but there was a kiddo who asked if I would stay. Anyway, these kiddos touch your heart.
From the participants’s point of view, one of the biggest challenges—and benefits—is the treatment environment itself. It’s in the middle of nowhere.”
About three weeks later, I met another field staffer who’d been doing the same thing for a long time before I did. She understood what it was to work with children in the wilderness who have all these difficulties. I ended up marrying her about six months later.
That was 30 years ago and we’ve [since] had six of our own children. We’ve probably had 3,000 kids behind us in terms of those who we’ve participated in providing treatment for. It’s just been wilderness therapy this whole time. My wife [Sheri] and I and a couple other people founded WinGate about 13 years ago.
Q: How do you explain wilderness therapy to families who are new to this concept?
Wilderness therapy became known as a powerful thing back in the late 1980s for private pay and adolescence. But all the way back in the 1960s, it was discovered at Brigham Young University to be very powerful in helping young people who were failing in college to get back on their feet, whether it be emotionally or because of addiction issues. That same model or pieces of it were brought forward into the 1980s. Wilderness programs started to come up and kind of proliferate. We’ve been with it from the beginning.
Q: Why do you think WinGate is uniquely successful in treating addiction?
A: There are a lot of reasons why people struggle with addiction. There is no addiction without previous trauma. If you want to successfully treat addiction issues, at some time or another you need to address trauma issues. In some cases, these trauma issues have to do with just the individual; in [other] cases it’s with the whole system that the individual is within.
Even larger than that, epigenetically speaking, the whole trail of ancestry that they’ve been in.
So addiction in the individual is addressed without all the influences around them. When we go back to the substances, or go back to gaming or sexual addiction or gambling or whatever it is, usually there’s a trigger of some kind.

When you have participants in the wilderness, there are very few triggers in the first place. Our [program] is in the middle of nowhere. If we’re working with a 23-year-old who has had to struggle with Xanax or heroin and they say, “You know what, screw it—I’m out of here,” they have to hike for sometimes two days just to leave and figure out how to get out of the wilderness. Then they’re going to have to try to figure out how to get to a substance.
Sometimes we have young adults and even adolescents who do try to take off. With adolescents, they can’t just leave. With young adults, they can. But we don’t give them a ride. So, they walk and walk and walk and walk and walk. The whole time we’re encouraging them. We turn most of them around, actually. Then they continue their treatment.
You’ll have people who have a month or two later say, “Oh my gosh, I’m so glad it’s so damn difficult to get out of here because I would have blown it.”
Q: Can you describe your treatment approach and process?
A: We treat from ages 13 to about 28. They’re in [small] groups of up to about nine [participants]. Adolescent girls are separate from boys. Our young adults are co-ed. It’s a tiny social community where everybody knows each other and we know the nuances of each other’s problems.
It’s difficult to be in the throes of addiction and be completely grateful for life at the same time. You end up being grateful for life out there. It’s not easy. You don’t see a bed. You don’t even really see the inside of a vehicle or have any comfort to speak of the whole time.
With our style of wilderness therapy, it doesn’t have a lot of distracting things like coming into a facility and then going back into the wilderness, or rappelling or these more recreational sorts of deals. It’s just simply living in the desert and the silence that comes with that.
A lot of people, they want distractions because they don’t want to listen to their own voice, which sometimes can be negative at first. If you can stick with it long enough and work with somebody who will help you, your actual, authentic voice starts to come to the fore. And you’re like, “No, I am a good person.” “No, this is because this has happened to me.” “No, I really can overcome this.” As opposed to, “I suck.”
How can you just get to this very grateful quietude? It happens every single day. Everything is mindful. Everything is meditative.
If nobody has been introduced to the 12-step program, there’s an introduction that happens. They can work through steps three and four, and maybe a little bit more. Now they know there’s a whole community out there that is supportive.
Q: What treatment therapies does WinGate use?
A: Between our cluster of therapists, we have several. [They include]: somatic experiencing, dialectical behavior therapy [DBT] and motivational interviewing. It’s probably a dozen different things.
If the mechanism—in this case, I’m talking about the wilderness—has power in and of itself, then the modalities used by the therapist [are] not the powerful thing that’s happening. If I’m in rehab, there are treatment opportunities, group sessions and individual sessions. With us, it’s just happening constantly.
We’re also doing DBT, and we’re doing our group session or individual sessions. We have these different therapeutic modalities in the middle of all this, and the treatment approaches augment this environment.
It doesn’t happen immediately. It takes sometimes two or three weeks before it even starts. And then it just goes pretty fast from there.

Q: What are you working on innovating at WinGate?
A: One of the things we have found is that even though everything is very meditative and mindful in everything we do, we’re trying to make that more formal. Rather than just hiking, we sit down to help participants understand when you’re hiking: If you have this particular intention, this will be more helpful.
We’re initiating tai chi, qigong and yoga. Again, these are interjected with any experience.
[Some participants] come into the wilderness [who are] resistant—resistant to treatment, resistant to people and resistant to [their] own duty and [their] own goodness. We have refined over the years a way to drop that resistance. We call it engaging agency—or creating curiosity. Agency is the ability to choose a way of being, which is then followed by the ability to make other choices. We know that the defiant child or defiant adult pushes back by being defiant. A depressed person pushes back by diving deeper into depression. You name it, it’s kind of a version of pushing back.
I’ve actually circumvented the carrot and the stick. It’s not about the behavioral approach at that point. It’s about them making decisions based on getting a sense that people around them are people and not objects and not ways to facilitate their addiction or as obstacles to get around to get to their addiction patterns.
When these changes happen, we very ceremoniously make a big deal. We pull them aside, in beautiful little ceremonial places, and tell them: “You’ve overcome this trauma. You were directionless and had no goals. You’ve been talking about goals for the last three days. What do you want to accomplish?”
Q: What do you wish you could change about the industry as a whole?
A: It’s starting to change the way that I wish it would, which is this very expanded way of what treatment looks like. It’s beginning to open up. For many years, there was this wall between mental health treatment and addiction treatment. It seemed like these two shouldn’t mix, even though there are mental health counselors and there were therapists in addiction. Nuanced things like treating trauma, for example. The addiction world was like, “Whoa, what does that have to do with it?” Those two worlds are coming together.
I would add, let’s speed it up a little bit.
Also, some of the modalities that were used were completely defined by whatever insurance would reimburse. If the insurance says we only have 30 days, then we’re going to create this 30-day program.
There is this wider, bigger, more expansive way of treating this holistically. Could [insurance companies] please get on board with that? I would love for that to change.
Q: What is the No. 1 policy change you would make if you were in charge of the country’s laws and healthcare?
A: I would include wilderness therapy as an acceptable standard, a completely mainstreamed, accepted modality of treatment. It’s not right now. We are working on it. We have data that’s coming out as an industry, but for a while insurance companies would ask, “Do they have walls and beds?” If you don’t have walls and beds, they don’t recognize it as treatment.
Q: After, three decades in this field, what is your top treatment takeaway?
A: 1. Treatment of addiction is treatment of trauma. Those cannot be separated.
2) If somebody really knew how amazing they were, they would reduce their proclivity toward addiction.
3) Healing, even from addiction, happens in people only if it happens between people. It’s a relational thing. Even if the person it’s happening between may not be alive anymore.
Photos: WinGate Wilderness Therapy