The psychoactive drug is rapidly building credibility as a therapy that can work where others have failed
By Veronica L. Holyfield
Traditional treatment modalities for substance use disorder—from inpatient rehabilitation centers to the 12 steps and group therapy—aren’t successful for everyone. Compounding traumatic events, environmental influences or hereditary factors prevent some people from finding relief through “traditional” treatment practices.
This is where alternative approaches come into play. One such therapy that has been gaining traction is ketamine, a psychoactive drug that acts on the nervous system. Though it has been dismissed by some medical practitioners as a recreational drug—as more of a problem than a solution—it has demonstrated great promise for treating depression, post-traumatic stress disorder (PTSD) and also addiction.
As a 2018 study in Neuropharmacology states, “[K]etamine has attracted attention as a rapid-acting anti-depressant but other studies have also reported its efficacy in reducing problematic alcohol and drug use. … Ketamine has been shown to effectively prolong abstinence from alcohol and heroin in detoxified alcoholics and heroin dependent individuals, respectively. Moreover, ketamine reduced craving for and self-administration of cocaine in non-treatment seeking cocaine users.”
The Ascent of Psychoactive Therapies

Complex trauma, PTSD, major depressive disorder and addiction are along the spectrum of mental health issues that severely impact daily life and are intensely difficult co-occurring illnesses to treat. According to the U.S. Department of Veterans Affairs, about 8% of the U.S. population will have PTSD at some point in their lives. The National Institutes of Health, meanwhile, report that more than 23 million adults, or roughly 10% of the population, have struggled with problematic drug use. Additionally, a study based on the National Institute on Alcohol Abuse and Alcoholism’s National Epidemiologic Survey on Alcohol and Related Conditions (NESARC-III) showed that individuals with drug use disorders were 1.3 times more likely to experience clinical depression, 1.6 times more likely to have PTSD and 1.8 times more likely to have borderline personality disorder compared to people without drug use disorders.
Despite alarming rates of struggle, many people never reach out for help, and when they do, they have inconsistent or unsuccessful outcomes. Reworking trauma responses, rewiring addiction cravings and obtaining lasting, effective relief from mental health disorders takes time, and an unfortunate number of people don’t survive the cycle of struggle. Recently, however, psychoactive drugs such as ketamine—as well as psilocybin and LSD—have proved capable of delivering sustained relief in cases that appeared to be lost causes.
“From a subjective, experiential standpoint, ketamine’s phenomenological effects—sense of time, space, self, emotions, thoughts, ideas, beliefs—provide the client the ability to pause, step back, and observe negative behaviors without judgment of themselves,” says Leonardo Vando, M.D., medical director for Mindbloom, which specializes in ketamine-based therapy.
As one of the clinics at the forefront of psychedelic medicine, Mindbloom has been applying the neuroscience of ketamine since 2018 to help folks overcome an unhealthy relationship with substances, as well as treat anxiety, depression and PTSD. The dual benefit of behavioral change through neurochemical pathways and transformative subjective experience makes ketamine superior to other psychiatric interventions, Vando says.
Moving swiftly from the realm of the illicit to the clinically researched in controlled study groups, psychedelics such as ketamine are now being considered seriously for use in the most difficult and treatment-resistant cases of psychiatric disorders. In 2000, the Johns Hopkins Center for Psychedelic Consciousness Research began evaluating the capacity of substances like psilocybin to heal neural pathways formed around unhealthy and unwanted behaviors and traumatic experiences. The work has resulted in promising outcomes for smoking cessation and eating disorders, in addition to mental illnesses and substance abuse disorders.
Resistance to Ketamine
Ketamine, which has been used in veterinary medicine and surgical procedures in humans as an anesthetic due to its ability to block the NMDA brain receptor, has hallucinogenic, tranquilizing and dissociative effects. Similar in drug categorization to phencyclidine (PCP) and nitrous oxide, or laughing gas, ketamine’s therapeutic uses are expanding as a desire among both medical professionals and patients to step up research has grown significantly.
Leveraging a non-ordinary state of consciousness can be beneficial, and what a psychedelic does is change the whole way in which you see things.”
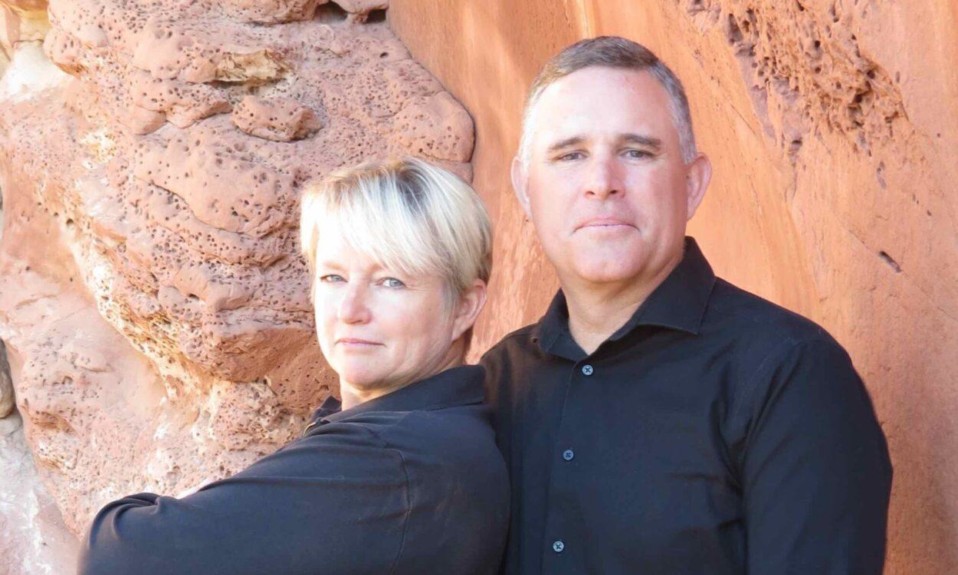
—Carl J. Bonnett, Klarisana
Yet not everyone is sold on ketamine. Carl J. Bonnett, M.D., founder and medical director of the ketamine psychotherapy organization Klarisana, says a primary source of resistance comes from the pharmaceutical industry due to the capitalist structure of traditional healthcare in the U.S. Moreover, he says, hardened negative views toward psychedelics, a result of the backlash against the 1960s-era counterculture that embraced them coupled with the War on Drugs that took hold in the 1980s, have affixed a stigma to psychedelics that makes them difficult to promote as a medical option.
“It’s actually quite ironic that what are derisively called primitive cultures have used mind-altering experiences for centuries, and now we come in with this puritanical overlay and say that the alteration of one’s mind categorically is bad,” Bonnett says. “You have to have the maturity to subdivide when it’s being done in a destructive manner versus when it’s being done in a personal development manner. Leveraging a non-ordinary state of consciousness can be beneficial, and what a psychedelic does is change the whole way in which you see things.”
Despite the pushback, ketamine is in Phase 2 of trials for Food and Drug Administration (FDA) approval for off-label use for psychiatric issues. Advocates for ketamine therapy believe it has the potential to provide the paradigm shift that many need in order to experience the healing that has eluded them.
Image: Shutterstock