The organization argues that virtual care has delivered results for those with OUD
By Jason Langendorf
Temporary policies allowing increased access to telehealth treatment for patients with opioid use disorder (OUD) during the COVID-19 pandemic should be made permanent, Pew Charitable Trusts recommended in a recently released issue brief directed at state lawmakers and Medicaid agencies.
Since the Coronavirus Aid, Relief and Economic Security (CARES) Act expanded access to telehealth (including addiction treatment) in March 2020, remote services have been embraced by an increasing number of patients, many of whom otherwise would have faced significant barriers to care. But the relaxing of these telehealth policies is tied to the federally declared COVID-19 national emergency, which is set to expire in February 2022.
Clinicians who used telehealth during the pandemic reported that it increased access and convenience for their patients, particularly among historically underserved populations.”
—Pew telehealth brief
Pew argues that telehealth-based treatment has benefited patients with OUD during the pandemic, and that telehealth outcomes have been comparable to those from in-person care. “Clinicians who used telehealth during the pandemic reported that it increased access and convenience for their patients,” Pew’s brief reads, “particularly among historically underserved populations such as people in rural or remote areas, people leaving incarceration, clients of syringe services programs and people experiencing homelessness.”
Pew’s Telehealth Access Recommendations
McKinsey & Company reported a massive spike in telehealth usage in April 2020—just after the passing of the CARES Act—followed by a gradual decrease and leveling off that had roughly plateaued since June 2020. But the report found that even as recently as February 2021, telehealth usage was at 38 times its pre-pandemic levels.
With increased telehealth access having proved both effective and popular, Pew is calling for permanent policy measures that will benefit more patients. These include:
- Requiring public and private insurers to reimburse OUD treatment providers for all services delivered via telehealth
- Setting public and private reimbursement rates for telehealth-based OUD services on a par with in-person treatment
- Expanding locations where patients can receive OUD treatment services via telehealth, including their homes
- Allowing patients with Medicaid to access OUD treatment services by telephone
- Enabling correctional institutions to use telehealth for OUD treatment services
Supporters of Telehealth Expansion
The permanent expansion of telehealth access and provisions has many supporters beyond Pew, both outside of and within Washington, D.C.
In July, a coalition of 430 healthcare organizations—including the American Health Association, the Mayo Clinic, Johns Hopkins Medicine and The Joint Commission—addressed a letter to U.S. Senate and House leaders calling for Medicare telehealth reform.
“Without action from Congress,” the letter stated, “Medicare beneficiaries will abruptly lose access to nearly all recently expanded coverage of telehealth when the Covid-19 [public health emergency] ends. This would have a chilling effect on access to care across the entire U.S. healthcare system, including on patients [who] have established relationships with providers virtually, with potentially dire consequences for their health.”
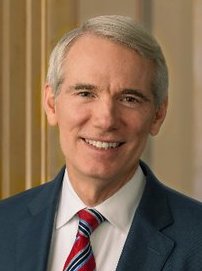
Last month, Sen. Rob Portman (R-Ohio) took to the Senate floor to advocate specifically for the benefits of telehealth addiction care, arguing that the spike in overdose rates during the pandemic would have been worse without more remote access and emphasizing the importance of permanently extending the current telehealth flexibilities.
“In the dark cloud of the pandemic,” Portman said, “the silver lining may be that we learn how to use telehealth better, and our legislation allows that to continue to be used with reimbursement, as an example [being] Medicaid reimbursement or Medicare reimbursement.”
Top photo: Shutterstock