The evidence shows that this dangerous form of addiction still needs to have a light fully shined on it
By William Wagner
March 11, 2021One of the biggest myths about eating disorders is that they’re a “female thing.” Not true. Eating disorders affect everyone—and they’re doing so in numbers much larger than previously estimated.
Just last week, an article published in The Lancet Psychiatry reported that the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2019 grossly underestimated the prevalence of eating disorders, to the tune of 42 million cases worldwide. The research revealed that eating disorders are four times more common than we thought, primarily because previous studies failed to account for the wide range of disorders beyond anorexia and bulimia
A corresponding commentary in The Lancet calls the new finding “stunning.” But Malcolm Horn, Ph.D., an expert in the field of eating disorders, isn’t surprised.
“Our society right now has so much disordered eating, where there are new diets, new fads,” says Horn, director of mental health services at the Rimrock Foundation, an addiction and mental health treatment provider in Billings, Mont. “It’s now so much easier to hide an eating disorder. It’s become socially acceptable to cut out entire food groups.
“And men often get missed. If a man loses a bunch of weight, a doctor might not think it’s an eating disorder. The doctor might say, ‘Oh, good job for exercising and eating better.’ Really, it might be that he’s not eating at all.”
Although an eating disorder is difficult to treat, the source often is surprisingly simple and intuitive: a lack of self-esteem.
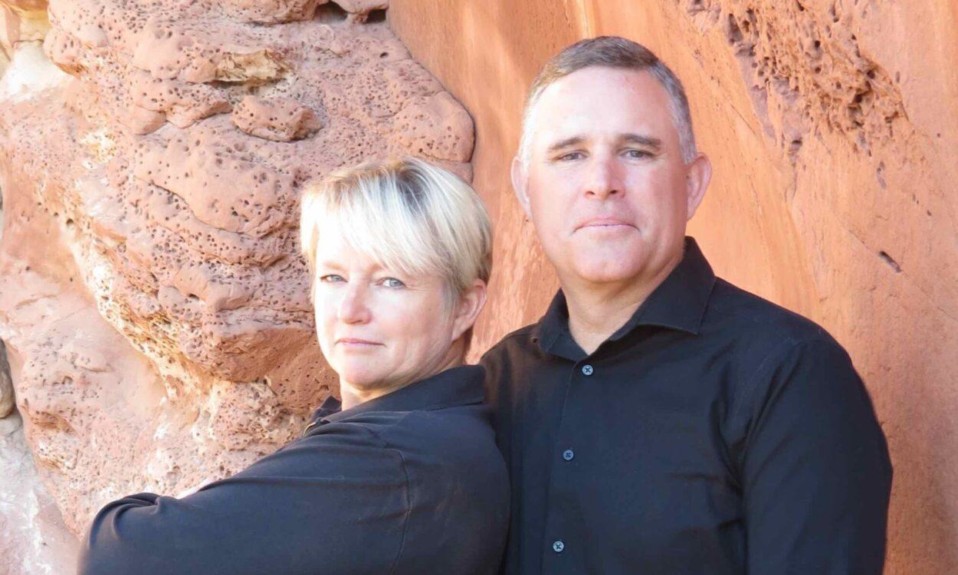
“There’s so much emphasis placed on someone’s appearance that if you add in some other factors, like depression or family dysfunction, you’re poking the bear,” says Robin Piper, CEO and clinical director of the addiction treatment center Turning Point of Tampa. “Someone mentioned their weight or how their body looks, and that comment was not necessarily meant to cause harm, but it was processed in that individual’s mind as, There’s something wrong with me, and now I have to change it. I have to be thinner; I have to be better. In order to do that, I have to eat less.”
Horn sums it up this way, based on a conversation she once had with a patient: “She said, ‘Cellulite is bad.’ I was like, ‘Why?’ She said, ‘If I have cellulite, no man is going to love me.’ I said, ‘Just so you know, the men don’t really care if you have cellulite. They’re just happy that you’re naked.’ So, it’s not about food—it’s about that belief system.”
Types of Eating Disorders
It’s also about addiction. An eating disorder is a disease in the same way alcoholism is. In fact, many people with an eating disorder suffer from co-occurring issues.
“A lot of people with eating disorders have very obsessive-compulsive-type qualities—just like with addiction to drugs or alcohol,” Piper says. “Probably three-quarters of our eating disorder population [at Turning Point] also has a coexisting condition with alcohol or drugs.”
Someone who’s bulimic might also go through a period of restricting their food significantly. And even someone with [binge-eating disorder] can go through a period of time where they’re purging their food. There’s a lot of going back and forth on that continuum of eating disorders.”—Robin Piper, CEO and clinical director, Turning Point of Tampa
Making matters stickier, not all eating disorders are created equal. Among the types of eating disorders are:
Anorexia nervosa: An obsession with being “thin” causes anorexics to take drastic measures, ranging from severely restricting their food intake to using laxatives or forcing themselves to vomit. It’s the most lethal eating disorder.
Bulimia nervosa: The life of a bulimic is a rollercoaster of binge-eating and then purging. Piper calls bulimia “the most common one we see [at Turning Point].”
Binge-eating disorder: Unlike with bulimia, there is no purging element. The end result is thus obesity.
Pica: The afflicted in these cases crave things that aren’t considered food, such as dirt or chalk.
Rumination disorder: Relatively newly recognized on the roster, rumination disorder involves regurgitating food.
Avoidant/restrictive food intake disorder (ARFID): Children under age 7 are most commonly diagnosed with ARFID, which is defined by a lack of interest in eating.
The various eating disorders don’t always exist neatly in separate buckets. Says Piper, “You go to the three major groupings [anorexia, bulimia and binge-eating], but most eating disorder clients kind of travel amongst those. They don’t just stay in one category. So, someone who’s bulimic might also go through a period of restricting their food significantly. And even someone with [binge-eating disorder] can go through a period of time where they’re purging their food. There’s a lot of going back and forth on that continuum of eating disorders.”
Treating Eating Disorders
Because of the disease’s slipperiness and its co-occurring aspect, clinicians face tricky work in untangling an eating disorder. The key, says Horn, is to develop an individualized treatment regimen for each patient. After all, even healthy bodies come in many shapes and sizes.

“What exactly do they need?” Horn says. “Finding that balance is difficult. You want them to focus on getting away from the numbers. It doesn’t matter how much you weigh. Who cares? Weight is not a very good indicator of overall health—it’s more about your bloodwork. How do you feel in your body? Do you feel comfortable? Do you feel relaxed? Are you beating up on yourself?”
Piper says Turning Point puts a team into action to provide that wellness approach: a nutritionist, a psychiatrist, a therapist with expertise in body issues, plus alcohol and drug clinicians if necessary. In theory, at least, patients then have the wherewithal to keep on keepin’ on once they venture out of treatment and back into the wild.
“They’re doing their own grocery shopping, their own meal prep, their own menu planning,” Piper says. “They have their hands in it, so to speak. When they leave the treatment environment, they know what to do. There’s no time to figure it out when they get out there in the real world. And they have the 12 steps built in, so they have support for the transition.”
Turning Point is among only a handful of programs that are fully geared for treating both eating disorders and alcohol and drug addiction. The scarcity of such programs means root problems aren’t addressed for many patients.
“They go into treatment [for alcohol] and a lot of times think, Okay, I’ll get sober, but I’ll still do the binging and purging [with food],” Horn says. “Sometimes treatment programs might not even be aware that’s happening, because it’s not on the radar. Then they get out of treatment, and, yep, they’re sober. But five years later, they have to go to treatment because of an eating disorder.”
Horn looks to the day when the treatment equation is complete. “In the future,” she says, “maybe both will just be the standard of care, and treatment facilities will do that automatically. They’ll have both of those abilities because they’ll understand they go hand in hand.”
Top photo: Helena Lopes