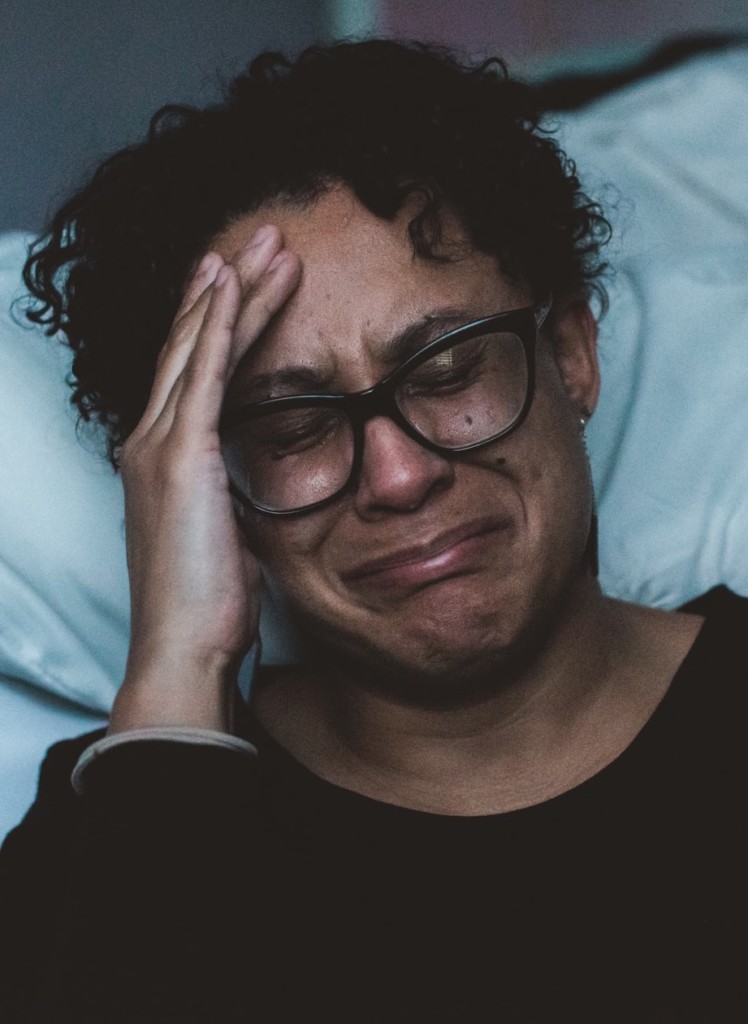
Things aren’t getting any easier for a population that has been hit hard by the pandemic
By William Wagner
The COVID-19 pandemic has been particularly brutal on people with addiction. And even in the “vaccine era,” that hasn’t changed much.
According to a study led by the National Institute on Drug Abuse (NIDA) and Case Western Reserve University that was published on Oct. 5 in the journal World Psychiatry, individuals with substance use disorders (SUDs) are significantly more vulnerable to breakthrough COVID infections. In their study, the researchers determined that 7.0% of vaccinated people with SUD had breakthrough infections, as opposed to 3.6% of vaccinated people without an SUD. They reached their conclusions by dissecting the health records of about 580,000 people in the U.S. with and without SUD who were fully vaccinated against the virus between Dec. 1, 2020, and Aug. 14, 2021.
It is important to continuously evaluate the effectiveness of COVID-19 vaccines and the long-term effects of COVID-19, especially among people with substance use disorders.”
—Rong Xu, Case Western Reserve University
“From previous studies, we knew that people with substance use disorders may be particularly vulnerable to COVID-19 and severe related outcomes,” Rong Xu, Ph.D., a professor at Case Western’s Center for Artificial Intelligence in Drug Discovery, said of the study. “It is important to continuously evaluate the effectiveness of COVID-19 vaccines and the long-term effects of COVID-19, especially among people with substance use disorders.”
Nora Volkow, M.D., director of NIDA, stresses that while the findings are troubling, they should in no way deter people with SUD from getting vaccinated.
“First and foremost, vaccination is highly effective for people with substance use disorders, and the overall risk of COVID-19 among vaccinated people with substance use disorders is very low,” Volkow said. “We must continue to encourage and facilitate COVID-19 vaccination among people with substance use disorders, while also acknowledging that even after vaccination, this group is at an increased risk and should continue to take protective measures against COVID-19.”
Before Breakthrough Infections
Even before the vaccine entered the picture, people with SUD were at greater risk of being devastated by COVID, mostly because heavy drinking and drug use eats away at the immune system. Lorenzo Leggio, M.D., Ph.D., M.Sc., senior investigator for the joint National Institute on Alcohol Abuse and Alcoholism (NIAA)-NIDA Section on Clinical Psychoneuroendocrinology and Neuropsychopharmacology, laid it out in an interview with TreatmentMagazine.com in September 2020:
“Patients with alcohol and substance use disorders do have an increased risk of infections—not just COVID but infections in general,” Leggio said. “In part, this is because alcohol and drugs damage the immune system. They make your immune system vulnerable, which increases your risk of getting infections.
“To make things more complicated, these are patients who also may have medical problems to begin with. For example, patients with addiction often have riskier [behaviors]; think about smoking. Also, they tend to be more prone to cardiovascular problems, including hypertension and heart issues. Other organs are damaged, too. And then when they get an infection—compared to someone who’s healthy—they have multi-organ medical problems. The body is less able to fight against the virus, and this leads the body to be more susceptible to complications from it.”
It stands to reason, then, that the vaccine is less effective for those with SUD. “Though vaccines are highly effective against COVID-19, their effectiveness in individuals with SUDs might be curtailed by compromised immune status and a greater likelihood of exposures, added to the waning vaccine immunity and the new SARS-CoV-2 variants,” states the World Psychiatry study.
Another Log on the Fire
Numerous studies have noted a spike in the use of alcohol and other substances throughout the pandemic. Much of the increase can be traced to psychological factors—notably isolation, which is among the greatest enemies for people with addictive tendencies and mental health issues.
“Some people might have already been struggling with mental health problems [before the pandemic],” says Michael Zvolensky, Ph.D., director of the University of Houston’s Anxiety and Health Research Laboratory/Substance Use Treatment Clinic. “For that certain subgroup, COVID probably brought out clinically significant distress. Many people [in the general population] will recover just fine, but a subset won’t. We don’t know the exact percentage, but a subset won’t without intervention or targeted care. It’s not that it can’t be treated, but we’ll have to roll out targeted public health efforts to address this need.”
Breakthrough infections are just one more obstacle to surmount in the seemingly never-ending battle against COVID’s effects.
Top photo: Engin Akyurt; bottom photo: Claudia Wolff














