The health company emocha is seeking to improve outcomes with a smartphone app that brings in-person medication monitoring to a video setting
By: Mark Mravic
Can a selfie help ensure that opioid use disorder (OUD) patients are taking their meds? That’s the idea behind Baltimore mobile health company emocha’s smartphone app, which is featured in several research studies as well as limited clinical practice.
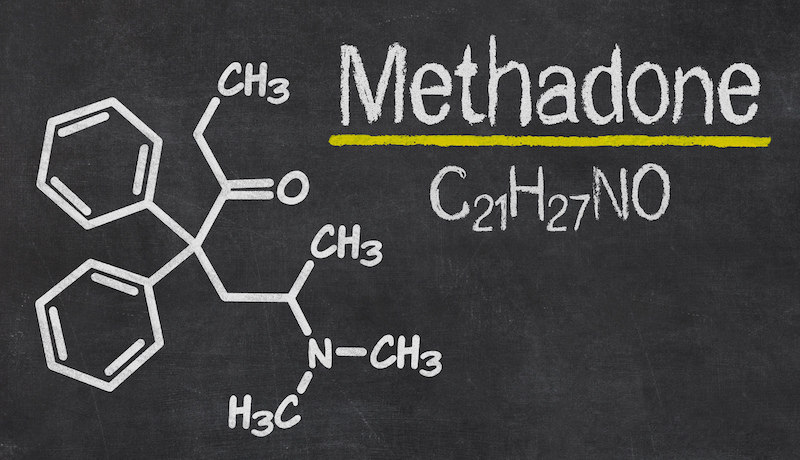
Adherence to medication-assisted treatment (MAT) is critical to recovery, but the percentage of people sticking with their meds remains a major concern. A 2018 study in Substance Abuse and Rehabilitation characterized buprenorphine adherence as “low,” finding that it hovered at only around 40% for the year after patients begin treatment. Factors that play into failure to keep up with treatment include cost, insurance coverage, dose size, co-occurring substance and alcohol misuse, and mental health issues. Research on methadone has yielded similar results—in one study, just 35% of patients remained on the medication for 12 months.
One effective tool is directly observed therapy (DOT). … Buprenorphine, however, is a take-home med that doesn’t require daily in-person monitoring. That’s the gap the emocha app is meant to close—using video directly observed therapy (VDOT) to mirror the in-person experience.”
Boosting adherence is critical to the success of MAT, since non-adherence is directly associated with relapse and can be a sign of misuse. So, how to raise the rate? One effective tool is directly observed therapy (DOT), in which patients come into a provider’s office and have their medication administered in person, under the watchful eye of a healthcare worker. This has been the standard of care for methadone. Buprenorphine, however, is a take-home med that doesn’t require daily in-person monitoring. That’s the gap the emocha app is meant to close—using video directly observed therapy (VDOT) to mirror the in-person experience.
The technique has proven successful in other indications, such as tuberculosis and hepatitis C, with adherence in the former case at better than 90% in one study—higher even than in-person observation, with lower costs and significantly better acceptance by patients. “We’ve proven that our platform secures the same rates of adherence as in-person DOT,” emocha CEO Sebastian Seiguer told The Baltimore Sun, “and we’ve done that in tuberculosis, and we’re doing it now in hepatitis C, where each dose of medication is several hundred dollars.”
VDOT has shown promise for substance use disorder (SUD) as well. A 2020 study in the Journal of Addiction Medicine of patients being treated for methamphetamine addiction with bupropion reported that 87% of dispensed doses were confirmed via video and in-person observations. Participants mostly appreciated that they didn’t have to come into the office for their meds, and staffers reported confidence that the information they were collecting was accurate. As that study noted, “Participant-level buy-in of the video-dosing component is clearly an important factor to adherence.”
It makes sense, then, to apply the technique to treatment for opioid addiction, an overarching healthcare crisis. “In opioid addiction,” according to Seiguer, “we can really help patients stay on a treatment plan and get better and recover from an addiction.”
How emocha Works

August Holtyn, Ph.D., assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, is currently involved in two research studies employing the emocha app. In both, participants use the technology to video themselves taking their medication, then send the footage to the research team as verification that they’re adhering to treatment.
Holtyn’s team has a step-by-step process, all on camera, for verifying that participants are taking the meds. “We observe them opening their buprenorphine film or packaging, and then we watch them take the film out of the package,” Holtyn says. “They put the film under their tongue, and they have to video record with the dose under their tongue for at least three minutes.” That length of time helps guard against diversion. “It’s likely [the medication] is going to be dissolved enough at that time that they wouldn’t be able to remove it from their mouth and give it to someone else.”
In addition, participants in one of the studies are using the app to perform and submit their own saliva drug testing. Holtyn’s team sends them point-of-care saliva-testing devices, and observes them opening the packages, swabbing the inside of their mouth and inserting the swab into the testing device. “We can watch the test processing on screen,” she says, “and then we read whether the test was positive or negative. And they do all that testing while recording the video using the app.”
If that sounds a bit complicated, remember that most people using smartphones these days know how to download an app and take a video selfie. “Participants pick up on how to use the app fairly quickly,” Holtyn says, “and the majority of them don’t have any issues with submitting videos.”
As with everything else, COVID has thrown Holtyn’s group a wrinkle: Before the pandemic, researchers brought participants in to instruct them on the process of using the app. Beginning last spring, however, they had to switch the on-boarding to be done remotely. “It can be a little hard when they’re on the phone with you, listening to your instructions, and you’re trying also to download and use the app,” Holtyn says. “But it’s been a pretty straightforward process.”
The Efficacy of the App
Because the studies are ongoing, Holtyn doesn’t have final results to report. Initial indications for the first study, involving people with OUD who were not in treatment before the program began, showed that adherence to the medication was about the same between app users and the control group. In contrast, the latter study, involving people already in buprenorphine treatment, had more promising preliminary findings. “With that population,” Holtyn says, “we’re getting high rates of app utilization. For our two groups that are engaging in buprenorphine adherence monitoring via the app, I’d say probably at least 90% of participants are submitting those daily videos.”
Just as COVID forced Holtyn’s team to adapt to a new situation, it disrupted treatment patterns on a broader scale. The pandemic created a special challenge for people with OUD who are being treated with methadone, since, as noted earlier, it required patients to show up daily at a clinic or other provider to receive their dose. With such levels of in-person contact impossible under COVID restrictions, the Substance Abuse and Mental Health Services Administration (SAMHSA) issued temporary guidance permitting the take-home use of the medication.
Our goal is to protect our patients’ safety while continuing to provide high-quality care, and emocha’s platform will enable us to do just that.”—Sean Soth, Evergreen Treatment Services
Given that leeway, Seattle-based Evergreen Treatment Services teamed with emocha last spring to use the company’s VDOT app to deliver services to its methadone patients. “Our goal is to protect our patients’ safety while continuing to provide high-quality care,” Evergreen director of clinical services Sean Soth said at the time, “and emocha’s platform will enable us to do just that.” Under such trying circumstances, the app would “protect patients and clinical workers while still ensuring high rates of adherence,” according to Seiguer.
To judge how emocha performed under these conditions, researchers at the University of Washington plan to conduct a retrospective study on the app’s effectiveness. In an earlier pilot study on buprenorphine, Judith Tsui, M.D., MPH, associate professor of medicine at UW, found that 93% of participants succeeded in using the app to confirm adherence to their daily buprenorphine regimen.
“The most important message here,” Tsui said, “is that patients can do this.”
Top photo: Nathan Dumlao